3891
Detection of recurrent prostate cancer with 18F-Fluciclovine PET/MRI1Department of Circulation and Medical Imaging, NTNU- Norwegian University of Science and Technology, Trondheim, Norway, 2St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 3Department of Radiology, St. Olavs Hospital, Trondheim University Hospital, 4Department of Nuclear Medicine, St. Olavs Hospital, Trondheim University Hospital, 5Ålesund sjukehus, Helse Møre og Romsdal HF, 6Department of Oncology, St. Olavs Hospital, Trondheim University Hospital, 7Department of Urology, St. Olavs Hospital, Trondheim University Hospital, 8Department of Cancer Research and Molecular Medicine, NTNU- Norwegian University of Science and Technology, Trondheim, Norway
Synopsis
Simultaneous PET/MRI has the potential to improve the detection accuracy in recurrent prostate cancer, since it combines the excellent soft-tissue contrast of MRI with the high molecular sensitivity of PET in one imaging session. The aim of this observational study is to assess the detection rate of recurrent prostate cancer by simultaneous 18F-Fluciclovine PET/MRI. We demonstrate that18F-Fluciclovine PET/MRI can detect suspicious lymph node, prostatic and bone lesions in patients with a wide range of PSA levels and that the number of equivocal findings is reduced when MR images are evaluated in conjunction with PET uptake. .
Purpose
Approximately one third of prostate cancer patients experience biochemical relapse (rising levels of prostate specific antigen, PSA) following initial treatment [1, 2]. Differentiating between loco-regional recurrence and distant metastasis at an early time point is crucial to provide proper treatment. There is growing evidence for improved biochemical control rates when salvage treatment is initiated at low PSA levels [3]. Unfortunately, currently recommended medical imaging methods (MRI and bone scintigraphy) lack sensitivity for detection of nodal and skeletal metastases at low PSA levels [4]. Simultaneous PET/MRI has the potential to improve the detection accuracy in recurrent prostate cancer, since it combines the excellent soft-tissue contrast of MRI with the high molecular sensitivity of PET in one imaging session. The aim of this observational study is to assess the detection rate of recurrent prostate cancer by simultaneous 18F-Fluciclovine PET/MRI. The performance of combined PET/MRI is compared to that of MRI-only, which is the current clinical standard.Materials and methods
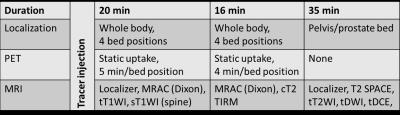
Patients that fulfilled the European Association of Urology criteria for biochemical relapse following radical treatment (two consecutive measurements with PSA ≥ 0.2 ng/ml following radical prostatectomy or PSA ≥ 2.0 ng/ml above the nadir following definitive radiotherapy [5]) and who were potential candidates for salvage treatment, were recruited and examined with simultaneous 18F-Fluciclovine PET/MRI (3 T Biograph mMR, Siemens, Erlangen, Germany). An overview of the imaging protocol is given in Figure 1.
MR images were reviewed by two radiologists blinded to the PET data. Subsequently, PET images were reviewed by a nuclear medicine physician with access to the initial results from MRI. Findings were scored as 1-negative, 2-equivocal or 3-recurrence/metastasis. A combined PET/MRI score was given after consensus between the reviewers. Detection rates for MR, PET and combined PET/MR are reported, calculated as the number of patients with suspicious findings divided by the total number of patients. Detection rates were divided into groups based on PSA level at time of imaging. Detection rates were compared with the chi-squared test. Median PSA levels in patients with and without suspicious PET findings were compared with the Mann-Whitney U test.
Results
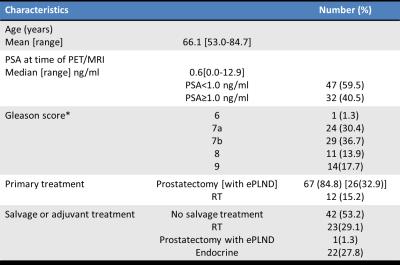
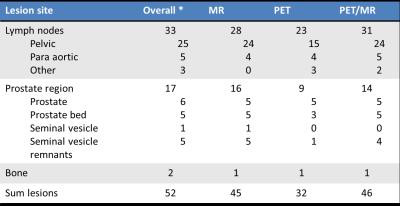
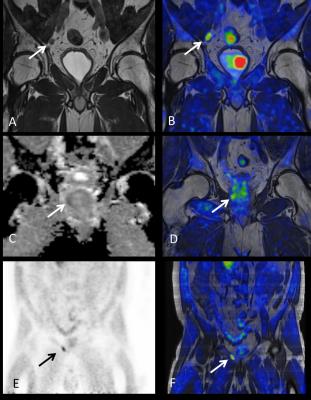
Patient characteristics (n=79) are listed in Table 1. In 53% of the patients there were no suspicious findings (negative score on MR, PET and PET/MR). In the remaining 37 patients there were 52 suspicious lesions (median 1, range 1-4 lesions per patient) in lymph nodes, prostate area and bone (Table 2)(Fig 2).
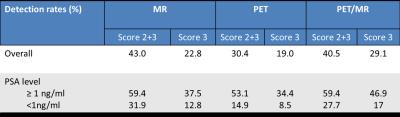
The detection rate for MR, PET and PET/MR were 43.0, 30.4 and 40.5% respectively when score 2 and 3 were considered positive. The PET/MR score was different from the MR score in 10 (12.7%) of the patients. Eight equivocal MR scores were changed to negative (score1, n=4) or positive (score 3, n=4) scores, while two negative MR scores were upgraded to equivocal (score 2, n=1) or positive(score 3, n=1) based on PET. When only considering score 3 as positive, PET/MR had higher detection rate than MR alone (29.1% vs 22.8% respectively, p<0.001)(Table 3).
Patients with PSA ≥ 1ng/ml had higher detection rates than patients with lower PSA levels at time of imaging (Table 3). Patients with elevated 18F-Fluciclovine uptake lesions (score 2 and 3) had higher median PSA level (2.2 ng/ml, range of 0.2-12.3 ng/ml), than PET negative patients (median PSA 0.5ng/ml, range 0-12.9 ng/ml)(p=0.001).
Discussion
We have demonstrated that simultaneous 18F-Fluciclovine PET/MRI can detect suspicious lymph node, prostatic and bone lesions in patients with a wide range of PSA levels. The overall detection rate is in the same range as previously reported for 18F-Flucoclovine PET/CT [6] and 11C-Choline PET-CT [7].
We observe that the number of equivocal findings is reduced when MR images are evaluated in conjunction with PET uptake. There were also cases of lesions with elevated tracer uptake that had been missed by the MR evaluation. This could indicate that a combined 18F-Fluciclovine PET/MR examination may play a role in detection of recurrent prostate cancer, and that the two modalities offer complementary information.
Although there is a higher detection rate among patients with PSA levels ≥1ng/ml, 18F-Fluciclovine PET/MR also detected suspicious lesions in patients with PSA as low as 0.2 ng/ml.
A limitation in this initial report is that there is no reference standard that can be used to categorize the findings as true or false positive. In future work, we aim to establish a reference standard based on PSA-levels, follow-up imaging, and lesion biopsies to define presence and absence of disease.
Conclusion
Combined 18F-Fluciclovine PET/MR can detect lesions suspicious for prostate cancer recurrence.Acknowledgements
No acknowledgement found.References
1. Freedland, S.J., et al., Time trends in biochemical recurrence after radical prostatectomy: results of the SEARCH database. Urology, 2003. 61(4): p. 736-41.
2. Zumsteg, Z.S., et al., The natural history and predictors of outcome following biochemical relapse in the dose escalation era for prostate cancer patients undergoing definitive external beam radiotherapy. Eur Urol, 2015. 67(6): p. 1009-16.
3. Ohri, N., et al., Can early implementation of salvage radiotherapy for prostate cancer improve the therapeutic ratio? A systematic review and regression meta-analysis with radiobiological modelling. Eur J Cancer, 2012. 48(6): p. 837-44.
4. Choueiri, T.K., et al., A model that predicts the probability of positive imaging in prostate cancer cases with biochemical failure after initial definitive local therapy. J Urol, 2008. 179(3): p. 906-10; discussion 910.
5. Heidenreich, A., et al., EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol, 2014. 65(2): p. 467-79.
6. Nanni, C., et al., 18F-FACBC compared with 11C-choline PET/CT in patients with biochemical relapse after radical prostatectomy: a prospective study in 28 patients. Clin Genitourin Cancer, 2014. 12(2): p. 106-10.
7. Krause, B.J., et al., The detection rate of [11C]choline-PET/CT depends on the serum PSA-value in patients with biochemical recurrence of prostate cancer. Eur J Nucl Med Mol Imaging, 2008. 35(1): p. 18-23.
Figures