3864
Respiratory motion-field reconstruction using low-rank plus sparse (L+S) approach for dynamic MRI of the lungs1Radiology, New York University, New York, NY, United States
Synopsis
A motion-guided low-rank plus sparse (L+S) approach for reconstruction of respiratory motion fields is presented for dynamic MRI of the lungs with high spatiotemporal resolution. Motion-guided L+S represents a paradigm shift where motion fields that describe deformations between respiratory phases are reconstructed instead of the respiratory phases themselves. The technique is demonstrated for normal and deep breathing imaging and compared against standard L+S reconstruction.
Purpose
Dynamic MRI of respiratory motion is a promising technique for functional evaluation of the lungs. However, low imaging speed of MRI severely limits spatiotemporal resolution and volumetric coverage if real-time imaging of respiratory phases is attempted. Recently developed techniques overcome these limitations by sorting or synchronizing data acquired during multiple respiratory cycles into respiratory phases, which are then reconstructed by either (a) weighting data consistency according to the respiratory phase – soft-gating approach (1-2) or (b) enforcing sparsity among respiratory phases – XD-GRASP approach (3-4). In this work, an alternative approach is proposed to reconstruct respiratory motion fields that represent the deformation from frame-to-frame instead of images using a motion-guided low-rank plus sparse (L+S) model (5). The proposed motion-guided L+S dynamic MRI is tested for continuously acquired 3D radial Ultra-short Echo Time (UTE) data acquired during normal breathing and heavy breathing and compared to standard L+S reconstructionMethods
A healthy volunteer was scanned on a 3T clinical scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen Germany) using a prototype 3D UTE sequence (6) with golden-angle rotation scheme based on the spiral phyllotaxis pattern. Relevant imaging parameters include: TR/TE=3.3/0.05ms, FOV=250x250x250mm3, 3D matrix size=256x256x256, voxel size=0.97x0.97x0.97mm3, and RF excitation angle=6o. The volunteer was instructed to breath normally for one minute, followed by consistent deep breathing maneuver for another one minute during which they were instructed to inhale as deeply as possible and exhale as rapidly as possible. These one-minute-normal and one-minute-deep breathing cycles were repeated for 4 times. Normal and deep breathing data were separated and individually sorted into 30 respiratory phases from expiration to inspiration and then back to expiration, covering an entire respiratory cycle using respiratory motion signal extracted directly from the data, as described in (4)
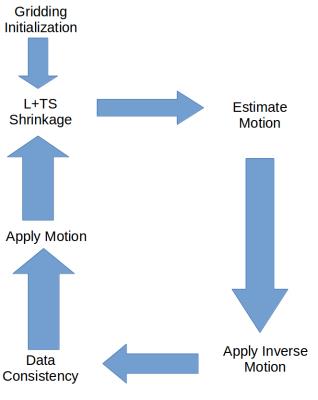
The reconstruction algorithms estimate the low-rank component L, transform sparse component S and motion fields B by solving the following optimization problem:$$\{L, S, B\} = \underset{L,S,B}{argmin} \frac{1}{2} \left \|y - A(L(B(x))+S(B(x)) \right \|_2^2 + \lambda_L \left \| L \right \|_* + \lambda_S \left \| TS \right \|_1,$$where $$$B(x)$$$ is the motion. We alternate between estimating the motion and an update of the cost function using the ISTA algorithm. Motion estimates were computed using pixel-by-pixel optical flow. Since the optical flow equations are underdetermined, we computed the minimum-norm solution followed by smoothing with a 3D Gaussian kernel, which exploits the fact that neighboring pixels usually have the same motion.
Figure 1 shows an overall flowchart of the algorithm, showing when the motion is estimated and applied in the data consistency step.
Results
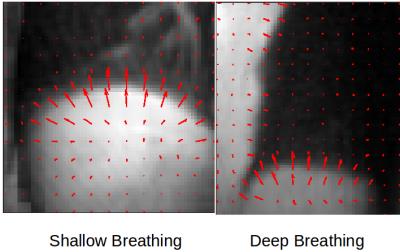
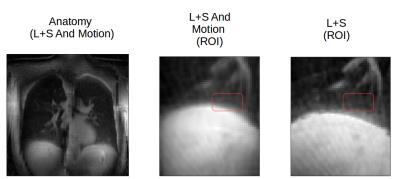
Figure 2 shows calculated motion fields for the shallow and the deep breathing case, with the motion vectors pointing in the correct motion direction of the diaphragm. Figure 3 shows the effects of motion compensation on temporal blurring of the diaphragm motion, with ghosting of the diaphragm being present when motion is not considered.Discussion
We have shown that incorporation of motion estimates into a low rank plus sparse reconstruction can lead to improved robustness of the reconstruction. Furthermore, our motion estimates are built directly into the reconstruction pipeline and thus improve the reconstruction by decreasing the rank and increasing the sparsity level of the reconstructed parameters. In the future we plan on incorporating more sophisticated model-based methods of motion estimation into the reconstruction pipeline to improve robustness. The estimation of respiratory motion fields provides spatially resolved quantitative information about pulmonary function, which can be potentially useful in clinical studies.Conclusion
Motion-guided L+S reconstruction is demonstrated for dynamic MRI of the lungs with improved performance over conventional techniques. The estimated motion fields not only guide the L+S reconstruction but provide quantitative information about respiratory motion, which can be used to assess lung function.Acknowledgements
No acknowledgement found.References
1. Chen J et al. JMRI 2015; 41: 460–473.
2. Jiang W et al. ISMRM 2016, 1139.
3. Feng L et al. MRM 2016; 75(2):775-88.
4. Feng L et al. ISMRM 2016, 2918.
5. Otazo R et al. ISMRM 2014, 742.
6. Delacoste J et al. ISMRM 2015, 1455.