3856
Comparison of Compressed Sensing Accelerated TOF MRA of the Neck with Conventional TOF MRA and Ultrasound in Clinical Cases1Diagnostic Imaging and Nuclear Medicine, Kyoto University, Graduate School of Medicine, Kyoto, Japan, 2Human Brain Research Center, Kyoto University, Graduate School of Medicine, Kyoto, Japan, 3Center for Advanced Imaging Innovation and Research (CAI2R) and Bernard and Irene Schwartz Center of Biomedical Imaging, New York University School of Medicine, Ner York, NY, United States, 4Siemens Healthcare GmbH, 5Siemens Medical Solutions USA, Inc.
Synopsis
Compressed sensing (CS) can accelerate time-of-flight magnetic resonance angiography (TOF MRA) of the neck. The whole length of carotid arteries from the aortic arch to the skull base was scanned in 2 minutes with an acceleration factor of 7.5. Iterative reconstruction that exploits regularization in 3 spatial directions required less than 3 minutes on a GPU. The degree of stenosis at carotid bifurcation for 22 patients was subjectively evaluated on maximum intensity projection images. Results of CS accelerated TOF MRA and conventional TOF MRA were compared with stenotic rates measured by ultrasound, and showed an excellent correlation.
Introduction
Carotid stenosis is a silent disease caused by atherosclerosis, which results in distal embolism or critical reduction in cerebral perfusion. Non-contrast-enhanced time-of-flight magnetic resonance angiography (TOF MRA) can noninvasively examine patients for screening or follow-up of carotid stenosis. However, it requires a long scan time, 15:07 min to cover neck vessels from the aortic arch to the skull base for a fully sampled measurement. Compressed sensing (CS) is a promising acquisition and a reconstruction method that allows to reduce scan time significantly without significant loss of image quality1,2. In our study, we used CS to reduce the duration of MRA scans of the neck by approximately a factor of 7 to 2:12 min (Fig. 1). However, largely under-sampled images reconstructed with CS can have degradation in image quality and therefore may result in over- or under-estimation of the stenotic region. Thus, we investigated the feasibility of CS TOF MRA in clinical cases of the neck by comparing it to conventional TOF MRA and ultrasound (US) for evaluation of carotid stenosis. US was considered as a reference because it can locally apply a US probe and quantitatively evaluate the stenotic rate.Materials & Methods
This study was approved by our institutional review board. Twenty-two patients (mean age, 71.7 years; range, 35 – 84 years; 16 men, 6 women) who received neck MRA and US within one month were enrolled. Imaging was performed on a 3T scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) with a 20-channel head-neck coil. TOF MRA scans were conducted using both conventional and CS prototype sequences with the following matched parameters: TR/TE = 20/3.69 ms, FA=18°, FOV = 220 × 200 mm², 6 slabs, matrix = 320 × 288 × 228, and voxel size = 0.7 × 0.7 × 1.0 mm³. Conventional TOF MRA scan took 6:56 min with parallel imaging (PI MRA, GRAPPA with 2-fold acceleration). In the CS scan, k-space was sampled sparsely using a Poisson disk pattern with radially varying density3 and on average 7.5-fold undersampling, which took 2:12 min. CS MRA data was reconstructed online with the built-in GPU. Regularization was applied to the whole slab, i.e., including all 3 spatial directions for improved image quality. Details of the sparse undersampling and iterative reconstruction have been described in the previous studies2-5. Each slab was separately reconstructed using iterations as soon as its acquisition was completed to speed up total reconstruction time. The degrees of stenosis at both sides of the carotid bifurcation were separately evaluated with maximum intensity projection (MIP) images on a 5-point scoring system (Fig. 2): 1, no stenotic change; 2, mild (<50% stenosis); 3, moderate (>50% stenosis without signal loss); 4, severe (>50% stenosis with partial signal loss); 5, occlusion (no signal). Stenotic rate was also measured by US with the Area method: 1, no stenosis; 2, mild (<50%); 3, moderate (>50% to <90%); 4, severe (>90% to <99%); 5, occlusion. These results were compared by using Spearman's rank correlation coefficient.Results
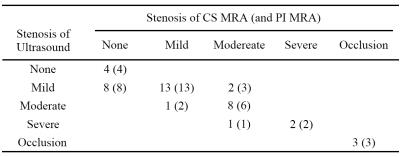
The reconstruction finished less than 3 minutes after the end of the acquisition. Two bifurcations were excluded because US could not be conducted due to metallic stent or severe calcification, and 42 bifurcations were evaluated. There was an excellent correlation between subjective scores evaluated with CS MRA or with PI MRA and quantitative stenotic rate evaluated with US (rho = .848 between CS MRA and US; rho = .809 between PI MRA and US, see Table 1). Among 15 cases with >50% stenosis in US, CS MRA underestimated in 2 (1, moderate as mild; 1, severe as moderate), and PI MRA underestimated in 3 (2, moderate as mild; 1, severe as moderate). On the other hand, no overestimations occurred.Discussion
CS could reduce scan time of neck MRA from 15:07 min to 2:12 min. This acceleration is much higher than that achievable with conventional methods, such as parallel imaging (6:56 min, 2-fold acceleration). The diagnostic capability of CS MRA with the higher acceleration was as good as that of PI MRA, and maintained an excellent correlation with US. Although several occurrences of false-negatives on mild stenoses were observed in both CS MRA and PI MRA, mild stenoses of carotid bifurcation were not actually important in clinical practice. Slab-by-slab reconstruction on the GPU enabled use of 3-dimensional regularization in clinically acceptable reconstruction time.Conclusion
TOF MRA of the neck can be highly accelerated by CS, while maintaining diagnostic capability.Acknowledgements
This work is supported in part by the Grant-in-Aid for Scientific Research on Innovative Areas “Initiative for High-Dimensional Data-Driven Science through Deepening of Sparse Modeling” (MEXT grant numbers 25120002, 25120008) of The Ministry of Education, Culture, Sports, Science and Technology, Japan.References
1. Lustig M, et al. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn Reson Med. 2007 Dec;58(6):1182–95.
2. Yamamoto T, et al. Time-of-Flight Magnetic Resonance Angiography With Sparse Undersampling and Iterative Reconstruction: Comparison With Conventional Parallel Imaging for Accelerated Imaging. Invest Radiol. 2016 Jun;51(6):372–8.
3. Stalder AF, et al. Accelerating TOF MRA in Clinical Practice using Sparse MRI with Variable Poisson Density Sampling. Proceedings of the 23rd Annual Meeting of the ISMRM, Tronto, Ontario, Canada; 2015. #3606.
4. Stalder AF, et al. Highly undersampled contrast-enhanced MRA with iterative reconstruction: Integration in a clinical setting. Magn Reson Med. 2015 Dec;74(6):1652–60.
5. Fushimi Y, et al. Compressed Sensing 3-Dimensional Time-of-Flight Magnetic Resonance Angiography for Cerebral Aneurysms. Invest Radiol. 2016 Apr;51(4):228–35.
6. Natsuaki Y, et al. Time-Of-Flight with Sparse undersampling (TOFu): towards practical MR applications of the Compressed Sensing. Proceedings of the 22nd Annual Meeting of the ISMRM, Milan, Italy; 2014. #0941.
Figures