3806
Dynamic Magnetic Resonance Imaging with Vaginal and Rectal Contrast for the Observation of Vaginal Vault and RectoceleHuici Zhu1, Jianyu Liu1, and Lizhi Xie2
1Radiology Department of Peking University Third Hospital, Beijing, People's Republic of China, 2GE Healthcare, MR Research China, BeiJing, People's Republic of China
Synopsis
To determine which method is better for the observation of vaginal vault and rectocele, this research compared the routine dynamic MRI with the dynamic MRI with vaginal and rectum contrast. There was statistically significant difference between the dynamic MR imaging and dynamic MR imaging with vaginal and rectum contrast. For the observation of vaginal vault prolapse and rectocele, the dynamic MR imaging with vaginal and rectum contrast was better than the routine method.
Purpose
Dynamic magnetic resonance imaging has been proven useful for evaluating pelvic floor dysfunction because it provides anatomic information about the muscles, ligaments, and sphincters, as well as functional information [1, 2]. To determine which method is better for the observation of vaginal vault and rectocele, this research compares the routine dynamic MRI with the dynamic MRI with vaginal and rectum contrast.Material and Methods
33 female PFD patients (mean age 60±9 years, eutocia, mean BMI 24.55, diagnosed by a urogynecologist with 30 years’ experience) underwent routine dynamic MRI and dynamic MRI with vaginal and rectum contrast successively on a 3.0T MR system (GE MR750). Before applying dynamic MR imaging, we filled the patient’s vagina and distal rectum with warm ultrasound (US) coupling gel, 20mL and 120mL respectively, using a flexible tube before the patient was moved onto the gantry. The patient was wrapped in an incontinence pad and covered with an absorbent towel to minimize discomfort from the eventual loss of urine and feces. The patient’s knees should be slightly parted so as not to interfere with organ prolapse. The MR imaging protocol began with a T1WI localizer sequence with a large field of view to identify the midline sagittal section, including the pubic symphysis, bladder neck, vagina, rectum, and coccyx. This sequence is followed by FRFSE T2WI in sagittal, axial and coronal planes (30 slices with 4 mm thickness, TR/TE=4500/100, FOV=22×22 cm, matrix=288×288, total imaging time=6’30’’minutes). For the dynamic study, a steady-state is applied in the midsagittal plane (FIESTA, 20 slices with 8mm thickness, TR/TE=3.6/1.5, FOV=34×34 cm, matrix=192×272), acquiring one phase per second. The patients were asked to evacuate contrast as dynamic MRI being obtained. Two observers (both of them have 10 years’ experience in female pelvic imaging diagnosis) evaluated the vaginal vault and rectocele on two dynamic MRI images, as well as applying MPL (mid-pubic) line to interpret dynamic MRI imaging (Figure 1). In the anterior compartment, the reference point is the most posterior and inferior aspect of the bladder base. In the middle compartment, the reference point is the most anterior and inferior aspect of the cervix. In the posterior compartment, the reference point is the anterior aspect of the anorectal junction. When a different opinion occurred, a uniform result is reached via discussion.Results
In routine dynamic MR imaging, the proportion of visibility of vaginal vault was 12.1% (4/33), the proportion of invisibility was 87.9% (29/33). In the dynamic MR imaging with vaginal and rectum contrast, the proportion of visibility of vaginal vault was 97.0% (32/33), the proportion of invisibility was 1.0% (1/33). Thus the two methods were statistically significantly different (p=0.00) (Figure 2). Furthermore, for the observation and diagnosis of rectocele, the dynamic MR imaging with vaginal and rectum contrast was better than the routine method (Figure 3). The application of MPL had contributed to the diagnosis of different degrees of pelvic organ prolapse and enterocele.Conclusion
Vaginal vault prolapse is the anatomical descent of the vaginal apex of middle vaginal compartment resulting from the disruption of its fascial supports. A rectocele is an outpouching of the rectal wall that protrudes onto the posterior aspect of the vagina, which can lead to outlet obstructive constipation [3]. Identification of vaginal vault prolapse and rectocele may facilitate both the surgical approach and repair [4]. However, the absence of reference point, the presence of atrophic changes, and the existence of previous pelvic surgery, all together make it difficult to observe the position of vaginal vault or diagnose rectocele. Our research applied the dynamic MR imaging with vaginal and rectum contrast, and made it possible to observe the vaginal vault and rectocele, which provided important anatomical information in preoperative diagnosis. In conclusion, for the observation of vaginal vault prolapse and rectocele, the dynamic MR imaging with vaginal and rectum contrast was better than the routine method, and it can provide reference for the determination of clinical operation method.Acknowledgements
No acknowledgement found.References
[1] Garcia dSL, de Miguel Criado J, Aguilera dHLF, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014. 34(5): 1417-39.[2] Taylor SA. Imaging pelvic floor dysfunction. Best Pract Res Clin Gastroenterol. 2009. 23(4): 487-503.
[3] Bitti GT, Argiolas GM, Ballicu N, et al. Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. Radiographics. 2014. 34(2): 429-48.
[4] Arbel R, Lavy Y. Vaginal vault prolapse: choice of operation. Best Pract Res Clin Obstet Gynaecol. 2005. 19(6): 959-77.
Figures
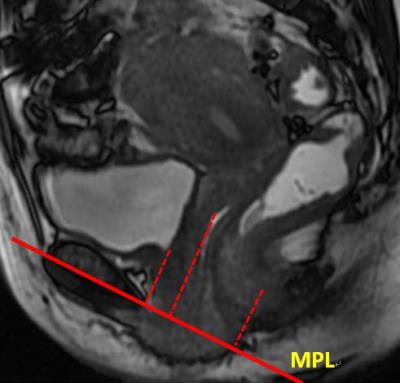
Figure.1 Sagittal FIESTA MR
imaging obtained at maximal strain. The distances from reference points (dotted
red lines) in the anterior, middle and posterior compartments to the MPL (solid
red line) are shown.
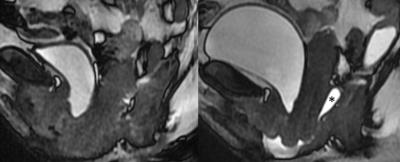
Figure.2 Sagittal FIESTA MR
imaging obtained at maximal strain. In the routine dynamic MR imaging(left),
the visibility of vaginal vault was unsatisfactory. In the dynamic MR imaging
with vaginal and rectum contrast(right), the visibility of vaginal vault was
satisfactory. (asterisk *)
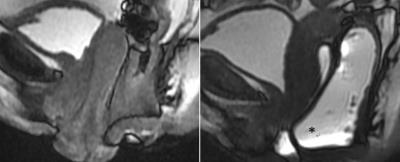
Figure.3 Sagittal FIESTA MR
imaging obtained at maximal strain. In the routine dynamic MR imaging(left), the visibility of rectocele
was unsatisfactory. In the dynamic MR imaging with vaginal and rectum
contrast(right), the visibility of rectocele was satisfactory. (asterisk *)