3659
Positive visualization of MR compatible nitinol stent using a susceptibility-based imaging method1Shenzhen Key Laboratory for MRI, Lauterbur Research Center for Biomedical Imaging, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, People's Republic of China, 2Centers for Biomedical Engineering, College of Information Science and Technology, University of Science and Technology of China, Hefei, People's Republic of China, 3Beijing Center for Mathematics and Information Interdisciplinary Sciences, Beijing, People's Republic of China, 4Department of Electrical and Computer Engineering, Texas A&M University, TX, United States
Synopsis
Previous studies have demonstrated that a susceptibility-based positive contrast MR method exhibits excellent efficacy for visualizing MR compatible metal devices by taking advantage of their high magnetic susceptibility. However, the method was not evaluated in the visualization of stents. Therefore, the purpose of this study is to assess whether the susceptibility-based positive method can be used to visualize the nitinol stents, with the comparison of two typical MR positive contrast techniques, i.e., SUMO and GRASP. Experiment results showed that the susceptibility-based method provides much better visualization and localization of the stent than SUMO and GRASP.
Introduction
MR-compatible metallic stents are commonly used
to treat arterial occlusive disease1. However, conventional MR
techniques have difficulty to accurately localize the stent position because of
the effects of susceptibility and radiofrequency (RF) shielding artefacts caused
by stent graft. Previous studies have demonstrated that a susceptibility-based positive contrast MR method
exhibits excellent efficacy for visualizing MR compatible metal devices (i.e., biopsy needle and brachytherapy seeds), by taking the advantageous of their high
magnetic susceptibility2,3. However, the method was never evaluated
in the visualization of larger devices such as stents. Therefore, the purpose
of this study is to prospectively assess whether the susceptibility-based method
can be used to visualize the nitinol stents, with the comparison of two typical
MR positive contrast techniques, i.e., susceptibility gradient mapping
using the original resolution (SUMO)
and the gradient echo acquisition for super-paramagnetic particles with
positive contrast (GRASP)4,5.Theory
Susceptibility-based positive contrast method: The method employed a modified 2D Fast Spin Echo (FSE) sequence to accelerate data acquisition3. Two datasets with and without readouts shifted (Tshift in the range of 0.2~0.7ms) are acquired for measuring the field induced by the nitinol stent. Thus, the amount of phase change induced by the local susceptibility difference between the stent and the surrounding tissues is accumulated during Tshift. After the data acquisition, a kernel deconvolution algorithm with a regularized ℓ1 minimization is used to calculate the susceptibility mapping and thus the positive contrast image of stent is realized.
SUMO: The method considers the local susceptibility gradient as an additional gradient which leads to an echo-shift in k-space for the signal affected by the susceptibility. Thus, a modified k-space filter can be applied into k-space to get the echo-shift and a positive-contrast image is then generated by a map of the strength of the susceptibility-gradient vector.
GRASP: The method can directly obtain the positive contrast image by a modified gradient echo sequence. As the signal in the region near the nitinol stent is conserved because the induced dipole field compensated for the dephasing gradient, a hyperintense signal is observed near the nitinol stent against the dark background.
Methods
Experiment: A tracheal stent (Ni-Ti alloy, 60mm ×20mm (length × diameter)) was perpendicularly placed into a gelatin phantom doped with 1.0 g/L copper sulfate solution, which was then positioned parallel to B0 and the axial and coronal multi-slice data were acquired. In the susceptibility-based method, two datasets were obtained with or without Tshift of 0.6 ms using the modified 2D FSE sequence. Scan parameters included: TR= 2000 ms, TE = 18 ms, slice thickness = 1.5 mm with no gap, and BW=134 Hz/Px. For SUMO, a 3D GRE sequence was used. Imaging parameters included: TR= 6.2 ms, TE = 2.5 ms, FA=15, slice thickness = 1.5 mm, BW=500 Hz/ Px. For GRASP, a modified 2D GRE sequence was used and the scan parameters are: TR= 11.5 ms, TE = 5 ms, slice thickness=2mm, BW= 130Hz/Px, the gradient rephasing was set to 50% of that used in the ordinary GRE sequence. All the three methods had the same in-plane spatial resolution of 0.67´0.67 mm2 and slice/partition number of 20.
Image analysis: To evaluate the positive contrast imaging results, the obtained positive contrast images were overlaid onto the corresponding magnitude images for qualitative comparison among the susceptibility-based method, SUMO and GRASP. Besides, the diameters of the stent were measured from the positive contrast images obtained by the three methods, respectively.
Results
All the three methods successfully realized
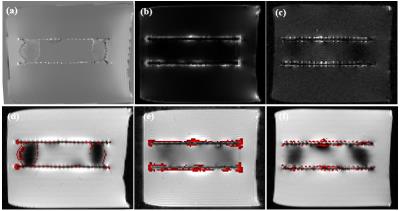
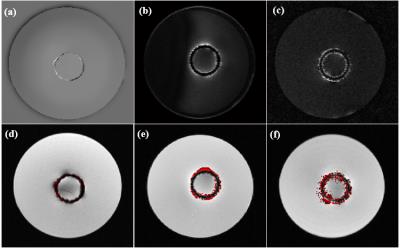
the positive contrast imaging of the nitinol stent (Figure 1&2). Compared
to SUMO (Figure 1b&2b) and GRASP (Figure 1c&2c), the
susceptibility-based method (Figure 1a&2a) could directly image the stent itself
rather than highlighted its surrounding susceptible area. The results of the positive
contrast images overlaid onto the magnitude images demonstrated that the
susceptibility-based method (Figure 1d&2d) could localize the stent more
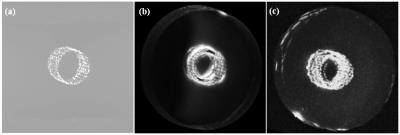
accurately than SUMO (Figure 1e&2e) and GRASP (Figure 1f&2f). Better visualization of the stent was also
realized by the susceptibility-based method than by SUMO and GRASP (Figure 3). According
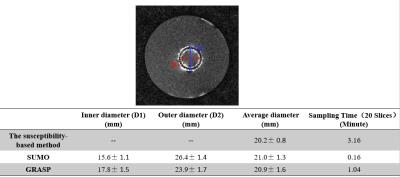
to the quantitative analysis, the measured diameter of the stent obtained by
the susceptibility-based method was 20.2
± 0.8mm, which was very close to the real one 20.0 mm (Table 1).Conclusion
Three positive-contrast techniques were
evaluated in this study. Compared to SUMO and GRASP, the susceptibility-based
method provides better visualization and localization of the stent. As the susceptibility-based
method can better visualize and localize the MR compatible metal devices, it
may have potential to be used in the MR-guidance interventional therapy, such
as the deep brain stimulation.Acknowledgements
This work was supported in part by the National Science Foundation of China (81328013, 81571669, 61201442, 81501463), National Science Foundation of USA (1606136), the National Key Research and Development Program of China (2016YFC0100302), and the Natural Science Foundation of Shenzhen (GJHZ20150316143320494, JCYJ20140417113430603, KQCX2015033117354154).References
[1] Lammer J, Bosiers M, Zeller T, Schillinger M, et al. First clinical trial of nitinol self-expanding everolimus-eluting stent implantation for peripheral arterial occlusive disease. Journal of Vascular Surgery, 2011, 54(2): 394-401.
[2] Dong Y, Chang Z, Xie G, Whitehead G, Ji JX. Susceptibility-based positive contrast MRI of brachytherapy seeds. Magn Reson Med, 2014, 74:716-726.
[3] Shi C Y, Xie G X, Zhang X Y, et al. Positive visualization of nitinol stent with susceptibility mapping using the Fast Spin Echo Sequence. ISMRM, 2016.
[4] Varma G, Clough R E, Acher P, Senegas J, Dahnke H, Keevil S F and Schaeffter T. Positive visualization of implanted devices with susceptibility gradient mapping using the original resolution. Magn Reson Med, 2011, 65: 1483-1490.
[5] Mani V, Briley-Saebo K C, Itskovich V V, Samber D D and Fayad Z A. Gradient echo acquisition for superparamagnetic particles with positive contrast (GRASP): sequence characterization in membrane and glass superparamagnetic iron oxide phantoms at 1.5T and 3T. Magn Reson Med, 2006, 55:126-35.
Figures