3565
Validation of Feasibility of Magnetic Resonance Imaging for the Measurement of Depth of Tumor Invasion in Distal Bile Duct Cancer1Korea University Anam Hospital, Seoul, Korea, Republic of
Synopsis
We performed the study to develop and validate a method for measuring the depth of tumor invasion (DoI) on magnetic resonance imaging (MRI) and to investigate the diagnostic performance of the measured DoI for stratifying T classification in patients with distal bile duct cancer. Our result showed that this newly developed method reliably measured DoI on T2-weighted MR images, and can be used for the preoperative T classification of distal bile duct cancer patients.
Purpose
It has been noted that the current tumor (T) staging system is associated with certain problems for both histopathologic and clinical aspects1~5. Several previous studies suggested an alternative T staging system using the depth of tumor invasion (DoI) to overcome the problems of the current T classification system 1,2,6. The purpose of this study is to develop and validate a method for measuring the DoI on magnetic resonance imaging (MRI) and to investigate the diagnostic performance of the measured DoI for stratifying T classification in patients with distal bile duct cancer.Methods
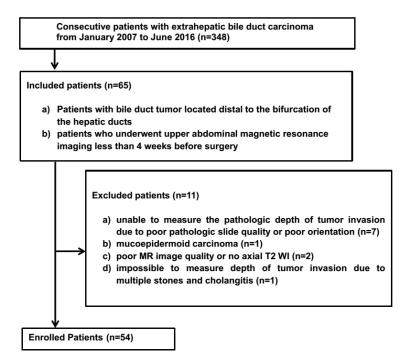
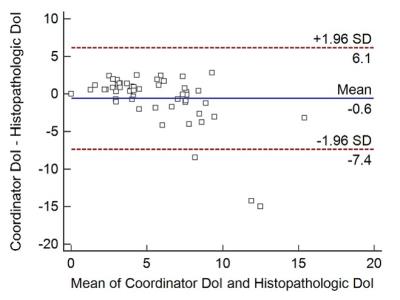
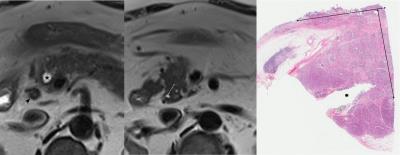
This retrospective study was approved by our institutional review board, and the requirement for informed consent was waived. Fifty-four patients (30 men, 24 women; age range, 43–81 years) with distal bile duct cancer who had undergone preoperative MRI participated in the study (Fig.1). A study coordinator developed a “provisional method” for measuring DoI based on published literatures and measured and measured the DoI of the included patients using the method. To overcome the defects of the “provisional method”, the coordinator and a pathologist reexamined MRI and histopathologic findings of outliers obtained from a Bland-Altman plot (Fig.2). The “Improved method” in MR based DoI measurement was determined to be useful after the introduction of supplement points. Two reviewers independently measured DoI and assessed its correlations with the histopathologic reference standard using intraclass correlation (ICC). To evaluate the diagnostic performance of MRI for T classification using DoI, the study population was radiologically and histopathologically divided into three groups according to the DoI.Results
The ICC between the DoI measured using the “improved method” and histopathologic DoI was very good or good (ICC coefficients 0.885 and 0.784, respectively), and the values were significantly higher than those obtained using the “provisional method” (ICC coefficient, 0.501; P = 0.00000 and 0.00075, respectively). The overall accuracy of MRI for stratifying bile duct tumors using DoI was 68.5% to 85.2%.Discussion
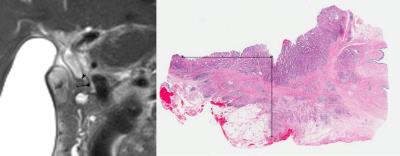
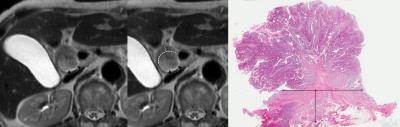
The “improved method” for measuring DoI on MRI was developed and was as follows; First, when the tumor shows a periductal infiltrating pattern and a low signal intensity epithelial lining is visualized overlying the tumor, the maximal distance between the epithelial lining and the outermost border of the tumor is measured (Fig.3); and when the tumor has an intraductal growing portion or when the low signal intensity epithelial lining is not visualized overlying the infiltrating tumor, an imaginary line connecting two break points of the dark signal intensity lining is used (Fig.4). Second, when there is a tumor component extension to the cystic duct, this portion is excluded for the measurement of DoI. Third, when the tumor signal intensity is indistinguishable from the adjacent pancreatic parenchyma and the abrupt narrowing site in MPD can be defined, the site of MPD obstruction was regarded as the outermost portion of the tumor in the measurement of DoI (Fig.5).Conclusion
The developed method for measuring DoI of distal bile duct cancer on MRI in our study can reliably measure DoI and stratify T-stage on T2-weighted images. Thus, MRI is a feasible tool for the preoperative T classification based on DoI and this may be helpful in predicting prognosis.Acknowledgements
No acknowledgement found.References
1. Hong SM, Cho H, Moskaluk CA, Yu E. Measurement of the invasion depth of extrahepatic bile duct carcinoma: An alternative method overcoming the current T classification problems of the AJCC staging system. Am J Surg Pathol 2007;31(2):199-206.
2. Hong SM, Kim MJ, Pi DY, et al. Analysis of extrahepatic bile duct carcinomas according to the New American Joint Committee on Cancer staging system focused on tumor classification problems in 222 patients. Cancer 2005;104(4):802-810.
3. Moon A, Choi DW, Choi SH, Heo JS, Jang KT. Validation of T Stage According to Depth of Invasion and N Stage Subclassification Based on Number of Metastatic Lymph Nodes for Distal Extrahepatic Bile Duct (EBD) Carcinoma. Medicine 2015;94(50):e2064.
4. Ebata T, Nagino M, Nishio H, Igami T, Yokoyama Y, Nimura Y. Pancreatic and duodenal invasion in distal bile duct cancer: Paradox in the tumor classification of the American Joint Committee on Cancer. World J Surg 2007;31(10):2008-2015.
5. Hong SM, Kang GH, Lee HY, Ro JY. Smooth muscle distribution in the extrahepatic bile duct: Histologic and immunohistochemical studies of 122 cases. Am J Surg Pathol 2000;24(5):660-667.
6. Min KW, Kim DH, Son BK, et al. Invasion depth measured in millimeters is a predictor of survival in patients with distal bile duct cancer: Decision tree approach. World J Surg 2016. In Press.
Figures