3551
Early Detection of Acute Pancreatitis (AP) Using MR Elastography (MRE) with Multislice Spin-echo Echo-planar Imaging1Shengjing Hospital, Shen Yang, People's Republic of China, 2People's Republic of China
Synopsis
An accurate early diagnosis(<24h of admission) of acute pancreatitis is clinically important. Our work shows that MR elastography has significantly better diagnostic performance for detecting AP than that achieved using the conventional CT/MR imaging, with improved sensitivity and accuracy. Early MRE is a promising technique to diagnose AP in a noninvasive fashion on admission.
Purpose
Acute pancreatitis (AP) is one of the most common reasons causing acute abdomen resulting in considerable morbidity and mortality 1. Early recognition of AP is essential for patient outcomes, so that suitable and prompt treatment can be provided. The diagnosis of AP remains problematic due to the lack of a gold standard diagnostic test. As described by the revised Atlanta classification 2, the diagnosis of AP requires two of the following three features: (1) abdominal pain consistent with AP; (2) serum lipase activity (or amylase activity) > 3 times the upper limit of normal; and (3) characteristic imaging findings. As atypical presentations, such as non-specific upper abdominal pain or normal to slightly elevated amylase (<3 times) are frequent at the admission in emergency room (ER) and there is a wide differential diagnosis, thus confirmatory tests are required for the final diagnosis of acute pancreatitis 3.In this study, our aim was to compare the diagnostic performance of MRE with conventional CT/MR imaging for early diagnosis of AP within 24 hrs of hospital admission.Methods
This is a cross-sectional prospective study involving 66 patients initially suspicious of AP who underwent both conventional CT/MR imaging and MR elastography within 24 hrs of admission. The diagnosis of AP was finally confirmed using the established diagnostic criteria (described by the revised Atlanta classification 2012)2. Of the 66 patients, 54 underwent CT and 12 underwent MRI. Twenty healthy individuals were included in the control group. All participants in control group had normal serum amylase and lipase levels, with normal pancreatic MRI findings.Pancreatic stiffness was measured and its diagnostic performance for AP was compared with that of conventional CT/MR imaging using receiver operating characteristic analysis with area under the curve (AUROC). MRE using a multislice echo planar imaging (EPI) sequence with a three-dimensional (3D) wave field inversion algorithm was used to generate pancreatic stiffness maps on a 3.0T GE scanner (Signa HDX 3.0T system; GE Healthcare, Milwaukee, WI). The imaging parameters were as follows: frequency=40Hz; TR/TE = 1375/38.8ms; phase offsets = 3; FOV = 40 cm; acquisition matrix = 96×96; number of signal averages = 1; frequency-encoding direction = RL; parallel imaging acceleration factor = 3; number of slices = 32; slice thickness = 3.5 mm.4Results
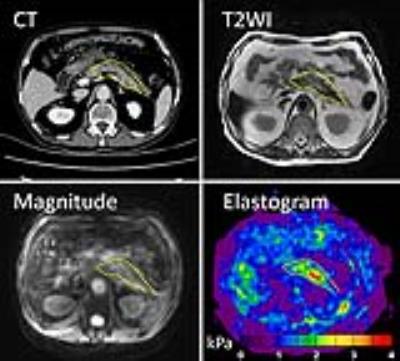
Finally 66 patients were included in this study, consisting of 46 patients with confirmed diagnosis of AP (AP group) and 20 patients without AP (non-AP group).The median pancreatic stiffness of 46 patients with AP was 1.97kPa (interquartile range [IQR], 1.69-2.85kPa), significantly higher than that of the 20 patients without AP (median [IQR], 1.19kPa [1.13-1.34] kPa).Typical AP cases are shown in Figure 1 and Figure 2. MRE (pancreatic stiffness >1.47kPa) showed significantly better diagnostic performance for detecting AP than that achieved using the conventional CT/MR imaging (AUROC: 0.981 vs 0.806, P=0.031), along with significantly improved sensitivity (96.2 % vs 76.1%, P<0.001) and accuracy (95.3% vs 80.9%, P<0.05). 11 AP patients with normal findings on early CT/MR had elevated stiffness. 3 non-AP patients that have slightly elevated pancreatic stiffness than the normal range(1.12kPa~1.39kPa).The combination of early MRE with the clinical criterion (2 of the 3 following criteria required:elevated stiffness higher than cutoff, typical abdominal pain and serum amylase and lipase 3 times higher than normal) at ER efficiently confirmed the early diagnosis of AP at initial hospital admission, with both 100% sensitivity and 100% specificity.
Discussion
Conventional CT/MRI is difficult to interpret at an early stage, especially in those patients with mild AP, little peripancreatic fat, or senile patients with atrophic pancreas, and negative findings was found in above 20% AP patients. In our study, 11 of 46 AP patients with early CT/MR scans revealed a normal pancreas, whereas all these cases had elevated stiffness. This finding suggests that MRE can successfully detect pancreatic mechanical changes quantitatively caused by early inflammation before visible morphological changes on conventional imaging. Acute inflammation causes edema, accumulation of inflammatory cells and interstitial liquid leading to changes of mechanical properties. MRE in the present study, was proved to be both sensitive and specific to identify these underlying pathophysiological changes. There are 3 non-AP patients that have slightly elevated pancreatic stiffness than the normal range of healthy pancreas. We speculate these patients might have unknown underlying chronic pancreatic diseases, such as latent chronic pancreatitis caused by alcohol abuse or habit smoking. Although slight increase, further studies are still needed to evaluate these confounding factors contributing to elevated pancreatic stiffness.Acknowledgements
We thank Richard Ehman and Kevin Glaser from the Mayo Clinic for providing the MRE system. We also thank Jun Chen from the Mayo Clinic for his assistance with providing the tailored pancreatic MRE driver.References
1.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-87 e1-3.
2. Lerch MM. Classifying an unpredictable disease: the revised Atlanta classification of acute pancreatitis. Gut. 2013;62(1):2-3.
3.Park MK, Jo J, Kwon H, et al. Usefulness of acoustic radiation force impulse elastography in the differential diagnosis of benign and malignant solid pancreatic lesions. Ultrasonography. 2014;33(1):26-33.
4.Shi Y, Glaser KJ, Venkatesh SK, Ben-Abraham EI, Ehman RL. Feasibility of using 3D MR elastography to determine pancreatic stiffness in healthy volunteers. J Magn Reson Imaging. 2015;41(2):369-75.
Figures