3547
PET/MR in pancreatic cancer: correlation between overall survival and functional imaging biomarkers from DCE-MRI, DWI, MR spectroscopy and PET1Department of Medical Imaging and Radiology, National Taiwan University Medical School and Hospital, Taipei, Taiwan, 2Department of Surgery, National Taiwan University Medical School and Hospital, 3Department of Internal Medicine, National Taiwan University Medical School and Hospital, 4Department of Nuclear Medicine, National Taiwan University Medical School and Hospital, 5Department of Oncology, National Taiwan University Medical School and Hospital, 6Departmen of Radiology, National Taiwan University Medical School and Hospital, Taipei, Taiwan, 7Department of Medial Imaging, Taipei City Hospital
Synopsis
The purpose of this study is to evaluate the association of imaging biomarkers from PET/MR with overall survival in pancreatic cancer patients. Sixty-four patients with pathologically-proven pancreatic adenocarcinoma underwent PET/MRI before treatment. The imaging biomarkers included Ktrans and Peak from DCE-MRI, minimal apparent diffusion coefficient from DWI, choline from MR spectroscopy, standard uptake values, metabolic tumor volume, and total lesion glycolysis of the tumors. Among all imaging parameters, Peak was found to be an independent predictor for overall survival in these patients. Thus, the imaging biomarkers from PET/MRI reflect different tumor characteristics and may predict survival outcome in these patients.
Introduction
The value of functional imaging parameters from positron emission tomography/magnetic resonance imaging (PET/MR) imaging for prediction of survival outcome in patients with pancreatic cancer is not well-known. The purpose of this study is (1) to understand the correlation among with the imaging biomarkers from PET/MR, including dynamic contrast-enhanced MRI (DCE-MRI), diffusion-weighted imaging (DWI), magnetic resonance spectroscopy (MRS), and glucose metabolic activity of PET; (2) to evaluate the association of these imaging biomarkers with overall survival in pancreatic patients.Materials and Methods
This prospective study was approved by the institutional review board and informed consent was obtained. Sixty-four consecutive patients with pathologically-proven pancreatic adenocarcinoma underwent PET/MRI before treatment. The imaging biomarkers were the Ktrans and Peak from DCE-MRI, minimal apparent diffusion coefficient (ADCmin) from DWI, choline level from MRS, standard uptake values (SUVmax and SUVpeak), metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the tumors. The relationships between these biomarkers were evaluated using Pearson correlation.By using the Cox proportional hazards model for univariate and multivariate analyses, the association of these imaging parameters and overall survival was investigated.
Results
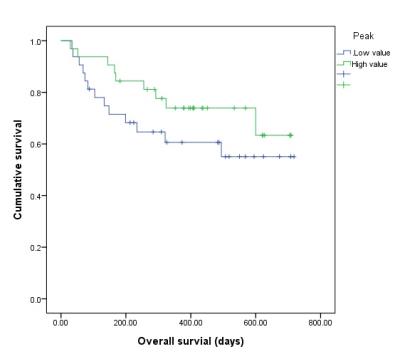
Peak was significantly negatively correlated with MTV (P=0.007) and TLG (P=0.015). ADCmin was significantly negatively correlated with SUVmax (P=0.029) and SUVpeak (P=0.012). Ktrans and Choline were not correlated with any other imaging parameters. Univariate analysis showed that patients with high Peak values seemed to have better overall survival (mean survival 560 vs 474 days), although not statistically significant (P=0.217) (Figure 1). However, Peak was found to be an independent predictor of overall survival (P = .032) after adjustment for age, sex, tumor size, stage, and other imaging biomarkers.Discussion
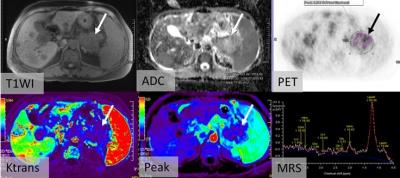
Our previous study1 found that the imaging biomarkers from integrated PET/MRI may predict clinical stage and progression-free survival (PFS) in patients with pancreatic or periampullary cancer, but whether these imaging biomarkers were associated with overall survival in pancreatic cancer patients remains unknown. In our previous study, The MTV/ADCmin ratio exhibited the highest AUROC for predicting T4, N1, M1, and advanced TNM stages tumors, and was an independent predictor of PFS (P = 0.018) after adjustment for age, sex, tumor size and stage. In this study, we found that tumor Peak value from DCE-MRI was an independent predictor of overall survival in patients with pancreatic cancer, and may better predict overall survival than other imaging biomarkers derived from PET/MR. A previous study2 showed that Peak represents a combination of blood flow, interstitial volume, and permeability within a tumor. Hence, it may reflect gross angiogenesis within a tumor. Previous studies2,3 also found a high pretreatment peak indicates longer overall survival in patients with advanced hepatocellular carcinoma which is consistent to our findings that high tumor angiogenesis suggests better overall survival. Thus, DCE-MRI may serve as a surrogate biomarker in predicting survival outcome or monitoring treatment response in these patients. Besides, we found that ADCmin was significantly negatively correlated with glucose metabolic activity on PET. Therefore, the information of these correlations between different imaging biomarkers may reflect different components within a tumor, including perfusion, flow, cellularity and metabolism (Figure 2).Conclusion
The imaging biomarkers from integrated PET/MRI reflect different tumor characteristics and may predict overall survival in patients with pancreatic cancer.Acknowledgements
The study is funded by National Taiwan University Hospital, Taipei, Taiwan; Contract grant number: A1 project No. NTUH103-A124. Ministry of Science and Technology (MOST) No. 104-2314-B-002-080-MY3
References
1. Chen BB e al. PET/MRI in pancreatic and periampullary cancer: correlating diffusion-weighted imaging, MR spectroscopy and glucose metabolic activity with clinical stage and prognosis. Eur J Nucl Med Mol Imaging. 2016 Sep;43(10):1753-64.
2. Chen BB et al. Dynamic Contrast-enhanced MR Imaging of Advanced Hepatocellular Carcinoma: Comparison with the Liver Parenchyma and Correlation with the Survival of Patients Receiving Systemic Therapy. Radiology. 2016 Nov;281(2):454-464.
3. Jarnagin WR, et al. Regional chemotherapy for unresectable primary liver cancer: results of a phase II clinical trial and assessment of DCE-MRI as a biomarker of survival. Ann Oncol 2009;20(9):1589–1595.
Figures