3545
Hyperpolarized [1-13C]pyruvate reveals increase of hepatic LDH activity following a glucose challenge in pigs1MR Research Centre, Aarhus University Hospital, Aarhus, DK, Aarhus N, Denmark, 2Department of Cardiology – Research, Aarhus University Hospital, Aarhus, DK, 3Department of Clinical Medicine - Research Laboratory for Biochemical Pathology, Aarhus University, Aarhus, DK
Synopsis
Hepatic regulation of glucose homeostasis is of pivotal importance and thus in vivo interrogation of hepatic energetic alterations in disease and treatment non-invasively using [1-13C] pyruvate has been proposed as a novel modality for assessing metabolic status. Here we investigated the metabolic effect of a glucose challenge on the porcine liver. A hepatic metabolic shift towards a reduced gluconeogenesis (increased lactate pool size) was observed following the glucose challenge, confirming hyperpolarized 13C MR’s ability to detect such changes. These findings support the use of hyperpolarized MR in metabolic challenge test in patients.
Purpose
To verify that Dynamic Nuclear Polarization (DNP) can be used as a method to quantify the hepatic metabolism in vivo in a porcine model following a glucose challenge. Dynamic nuclear polarization is a novel method allowing in vivo quantification of metabolism of [1-13C] pyruvate and into its metabolic products (alanine, bicarbonate and lactate)1. We hypothesis that following a glucose challenge the lactate dehydrogenase (LDH) and alanine transferase (ALT) will increase and that these changes are detectable by hyperpolarized 13C MR. Here we present metabolic data of the porcine liver that to our knowledge is the first hepatic DNP study of a larger animal model.Materials and methods
Twelve healthy Danish landrace pigs were included. All pigs were sedated with i.m. injection of a mixture of Stressnil (0.1 ml/kg bodyweight) and Midazolam (2.0 mg/kg bodyweight) for transport. Each pig received 120 mg of propofol (B. Braun Medical A/S) i.v. and was intubated and mechanically ventilated with a tidal volume of 300-425 ml and a respiration frequency ranging from 12-20 breaths per minute aiming at an end-tidal CO2 at 5.5 %. Anesthesia was maintained by 3% sevofluran mixed in atmospheric air with 40 % oxygen. To monitor blood pressure and to obtain blood samples, a 5fr. catheter was placed in the left femoral artery using ultrasound guidance. Additionally, two 5fr. catheters was placed in the femoral veins, one on each side, one catheter for administration of hyperpolarized [1-13C] pyruvate samples and one catheter for withdrawal of venous blood. Each pig received approximately 600 mg of [1-13C] pyruvate acid. A 3T GE Hdx MR-scanner (GE Healthcare, Milwaukee, WI, USA) was applied both for MRI and hyperpolarization spectroscopy. The integrated body coil was used for proton imaging. For 13C spectroscopy, the scanner was equipped with a bore-insertable 13C volume excitation resonator integrated in the patient table (GE Healthcare, Milwaukee, WI, USA). This was combined with a 16-channel flexible receiver heart array coil (Rapid Biomedical, Rimpar, Germany). Expiratory triggered hyperpolarized spectroscopy was done with 1 cm thickness oblique single slice covering the liver; repetition time approximately 1 s; total recording period 120 s; flip angle 10°. Blood samples were collected throughout the experiment. Hyperpolarized [1-13C] pyruvate was injected at 0, 20, 40 and 60 min. At 5 minutes, a bolus of 1g/kg glucose (glucose, 500 g/l; SAD, Copenhagen, Denmark) was injected intravenous. Normality was assessed with quantile plots. P<0.05 (*) was considered statistically significant. Repeated measurement analysis of variance (ANOVA) was used to compare the overall and individual metabolic and functional data.Results and discussion
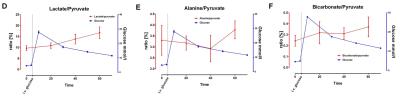
The main finding of this study was the acutely altered pyruvate-to-lactate conversion concomitant with a maintained pyruvate-to-bicarbonate conversion following a glucose challenge test in a postprandial large animal model. The blood glucose level (figure B) significantly (p<0.0001) increased over time peaking at 10 min after the first pyruvate injection. Insulin increased after glucose infusion with a peak at 70 min (p=0.03). Free fatty acid (FFA) levels decreased over time (P=0.004) figure C. The hyperpolarized data showed no significant change over time in alanine / pyruvate (p=0.54, figure E) or bicarbonate / pyruvate (p=0.62, figure F); however lactate / pyruvate significantly increased over time (p=0.02, figure D). The change from a fasted state to a hyperglycemic and hyperinsulinaemic state would be expected to decrease glycogenlysis and gluconeogenesis and increase glycogen synthase2. This could cause the pool size of lactate and alanine (yet in a lesser degree) to increase. This is because less lactate and alanine are converted to glucose via pyruvate due to the decrease in gluconeogenesis. This is supported by the recent studies by Lewies et al.(3,4) showing an increased lactate pool following metformin treatment (reduced gluconeogenesis). This is consistent with our findings of an increased LDH activity when FFA decreases and insulin level increases, interestingly it has been shown that metformin treatment increases gluconeogenesis under hyperglucagonemia5,6. Our findings support the reduced gluconeogenesis and consequently increased LDH activity when FFA decreases and insulin level increases in a normoglucagonemic state support the use of hyperpolarized MR to monitor the acute effect of alterations in metabolic pattern associated with fasting status and treatment response.Conclusion
We found that intravenous glucose injection and repeated pyruvate injections increase hepatic LDH activity, which has been shown to be related to altered gluconeogenesis and thus support hyperpolarized pyruvate as a method for in vivo quantification of glucose metabolism in the liver in a large animal model reassembling human physiology.Acknowledgements
No acknowledgement found.References
1. Ardenkjaer-Larsen, J. H. et al. Increase of signal-to-noise of more than 10,000 times in liquid state NMR. Discov. Med. 3, 37–39 (2003).
2. Roden, M. & Bernroider, E. Hepatic glucose metabolism in humans--its role in health and disease. Best Pr. Res Clin Endocrinol Metab 17, 365–383 (2003).
3. Lewis, A. J. et al. Assessment of metformin induced changes in cardiac and hepatic redox state using hyperpolarized[1- 13 C]pyruvate. Running title: Hyperpolarized MR assessment of metformin.
4. Madiraju, A. K. et al. Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature 510, 542–6 (2014).
5. Christensen, M. M. H. et al. Endogenous glucose production increases in response to metformin treatment in the glycogen-depleted state in humans: a randomised trial. Diabetologia 58, 2494–2502 (2015).
6. Konopka,
A. R. et al. Hyperglucagonemia mitigates the effect of metformin on
glucose production in prediabetes HHS Public Access. Cell
Rep 15, 1394–1400 (2016).
Figures