3430
Detection of Brown Adipose Tissue: Hyperpolarized 129Xe MRI vs Xenon Enhanced CT1Physics and Astronomy, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States, 2Biomedical Research Imaging Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States, 3Material Science, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
Synopsis
Despite histological evidence that all humans have brown adipose tissue, the detection of this tissue in overweight and obese subjects has proven to be a challenge. Here we demonstrate the combined used of hyperpolarized xenon gas (HP129Xe) MRI and xenon enhanced CT for the detection of BAT thermogenic activity and mass in lean and obese mouse phenotypes as well as our preliminary results in healthy young volunteers.
Introduction
Accurate
measurements of brown adipose tissue1 (BAT) volume and thermogenic activity remain
one of the major roadblocks to our understanding of the physiology and function
of this tissue in humans2. While 18F-FDG-PET/CT and MRI have both been used
to assess BAT tissue function and mass, partial volume effect and lack of
specificity have prevented accurate quantification of tissue mass and function2. Recently we have shown that magnetic resonance
with Hyperpolarized 129Xe gas (HP129XeMR) can be used to detect the presence of
this tissue and its thermogenic activity3. However, the resolution achievable with HP129XeMR
is far from what is needed to accurately quantify tissue mass. Here we show
that xenon enhanced CT (XECT), typically considered as an alternative to HP129XeMR,
can actually provide complementary information.Methods
A
total of 24 animals (12 lean and 12 ob/ob female mice) underwent XECT and
HP129XEMR studies. For the XECT studies, anesthetized animals were mechanically
ventilated either with a mixture of 70vol% N2 and 30vol% of O2 (non enhanced
scans), or with a mixture of 70vol% Xe and 30vol% of O2 (enhanced scan).
Enhanced scans were acquired before and after stimulation of thermogenic
activity, achieved by a subcutaneous injection of norepinephrine (NE at a dose
of 10mg/kg). Radio density enhancement was then used to quantify xenon
biodistribution. BAT areas were identified in CT images as areas that underwent
an increase in radiodensity of more than 50 Hounsfield Units (HU) after NE injection. Histology and
immunohistochemistry was also performed to correctly identify BAT regions. HP129XeMR
spectra were acquired by ventilating the animals with a mixture of 25vol% of O2
and 75vol% Xe, polarized up to 15% by using a commercial polarizer (PoLarean
Inc, Durham NC). Thermogenic activity in BAT was assessed by measuring the frequency
shift of the lipid-dissolved xenon resonance. Human XECT and 18F-FDG-PET images
were acquired on 3 normal weight young (age less than 30 y.o.) volunteers, by
using an hybrid PET/CT scanner (mCT, PET/CT Siemens Medical Solutions, Erlangen,
Germany). For these studies, subjects were exposed to mild
cold for 1 hour before the injection of 500mCi of 18F-FDG and for 60-70 minutes
before the acquisition of static 18F-FDG-PET images. XE images were acquired before and during
continuous xenon inhalation (concentration of 20-30%).Results
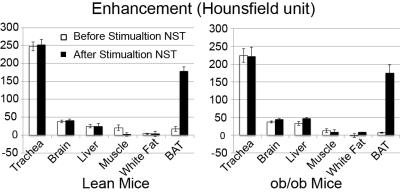
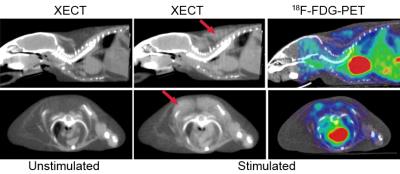
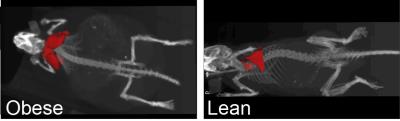
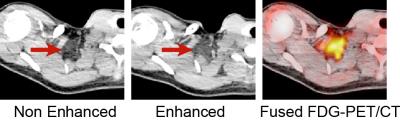
Figure 1 shows a comparison between XECT and HP129XEMRI as obtained in an obese mouse. Figure 2 shows the change in tissue radiodensity during xenon inhalation, before and during stimulation of thermogenic activity, in both lean and obese mice. An enhancement of more than 150 HU is observed in BAT of both lean and obese mice. Figure 3 shows representative XECT images before and during stimulation of thermogenic activity in an obese mouse and comparison with 18F-FDG-PET/CT on the same animal. The tissue is visible only after stimulation of thermogenic activity, even though glucose uptake is only slightly higher than glucose uptake in surrounding white fat. Figure 4 shows BAT segmentation in lean and obese mice. Figure 5 shows XECT BAT enhancement in one of the lean young subjects. The enhancement is restricted to areas with high glucose uptake, whereas it is absent in subcutaneous fat or in other regions of the supraclavicular fat depot, which would be typically assigned to BAT by fat fraction techniques.Discussion
XECT confirms our previous results obtained with HP129XeMRI showing that, during stimulation of thermogenic activity, xenon specifically accumulates in BAT and not in the surrounding white adipose tissue (WAT), in a concentration high enough to change tissue radiodensity by more than 150 HU, both in lean and obese mouse phenotypes. This strong change in tissue radiodensity allows for easy segmentation and quantification of BAT mass, even in the obese phenotypes in which BAT is undistinguishable from surrounding WAT. When xenon enhanced CT is combined with measurements of thermogenic activity performed by HP129XeMR, they reveal that reduction in tissue thermogenic activity is accompanied by tissue hypertrophy. Preliminary studies in humans mirror the results obtained in mice in that they show a specific enhancement of only few regions within the supraclavicular depot, thus confirming that not all supraclavicular fat is BAT. Specifically the enhancement, in the lean and young subjects analyzed here, is higher in areas with strong glucose uptake and absent in areas with low glucose uptake, as in the lean mouse phenotype.Conclusion
XECT and HP129Xe MR have always been seen as competing techniques. Here we show that XECT together with HP129XEMRI provide a complete picture of BAT, both from a functional and morphological standpoint.Acknowledgements
This work was supported by NIH grant number DK056350 and DK108231.
References
1. Cannon, B. & Nedergaard, J. Brown adipose tissue: function and physiological significance. Physiol. Rev. 84, 277–359 (2004).
2. Cypess, A. M., Haft, C. R., Laughlin, M. R. & Hu, H. H. Brown Fat in Humans: Consensus Points and Experimental Guidelines. Cell Metab. 20, 408–415 (2014).
3. Branca, R. T. et al. Detection of brown adipose tissue and thermogenic activity in mice by hyperpolarized xenon MRI. Proc. Natl. Acad. Sci. 111, 18001–18006 (2014).
Figures
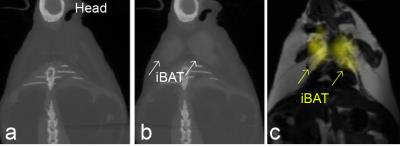
Comparison of XECT with HP129Xe MRI in an obese mouse. Despite fat fraction being similar to that of surrounding WAT before stimulation of thermogenesis, during stimulation specific accumulation of xenon in BAT dramatically changes the radiodensity of this tissue allowing its differentiation from surrounding white fat by both XECT and by HP129XeMRI. Even though HP129Xe MRI allows us to detect the presence of this tissue and to measure directly its temperature and thermogenic activity, its low resolution (1x1x10 mm3) prevents us from quantifying BAT volume.