3428
Inter-ethnic variation and SCD1 polymorphism predict risk for intramyocellular lipid accumulation in early childhood1Singapore Institute for Clinical Sciences, A*STAR, Singapore, 2Department of Obstetrics & Gynaecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 3Singapore BioImaging Consortium, A*STAR, Singapore, 4Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 5Department of Paediatric Endocrinology, KK Women’s and Children’s Hospital, Singapore, 6Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, 7MRC Lifecourse Epidemiology Unit & NIHR Southampton Biomedical Research Centre, University of Southampton & University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom, 8Clinical Nutrition Research Centre, Singapore Institute for Clinical Sciences, A*STAR, Singapore, 9Department of Endocrinology, Tan Tock Seng Hospital, Singapore, 10Department of Paediatrics, Faculty of Medicine, McGill University, Montreal, Canada, 11Department of Epidemiology, Biostatistics and Occupational Health, Faculty of Medicine, McGill University, Canada, 12Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital, Singapore, 13Liggins Institute, University of Auckland, Auckland, New Zealand, 14Department of Biochemistry, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Synopsis
A large intramyocellular lipid (IMCL) pool is associated with early pathogenesis of insulin resistance and type 2 diabetes. Studies from mother-offspring cohorts indicate that, like obesity and metabolic traits, IMCL is also highly heritable. However, here have been not many studies on the effect of genetic variation on IMCL. Although a number of genome-wide association studies (GWAS) have established associations between several genetic loci and metabolic disorders, it is not yet known if these loci also contribute to IMCL levels, and help explain ethnic difference in IMCL levels. In this study, we examined the ethnic differences (Indian, Malay and Chinese) in IMCL in Singaporean children and the genetic risk variant(s) associated with these differences.
Introduction
Skeletal muscle insulin resistance (IR) is considered to be the primary defect of type 2 diabetes mellitus (T2DM) and can precede the appearance of overt T2DM (β-cell dysfunction and fasting hyperglycemia) by decades [1]. A large intramyocellular lipid (IMCL) pool is associated with early pathogenesis of insulin resistance due to bioactive lipid intermediates that impede insulin signaling and insulin-mediated glucose uptake [2]. Genetics plays a significant role in the development of T2DM. Studies from mother-offspring cohorts indicate that IMCL is highly heritable, with maternal IMCL levels explaining 39% of the variance in offspring IMCL [3]. Certain ethnic groups, such as South Asians, are known to have a higher predisposition to metabolic diseases, as well as IMCL accumulation [4]. Although a number of genome-wide association studies (GWAS) have established associations between several genetic loci and metabolic disorders, it is not yet known if these loci also contribute to IMCL levels, and help explain ethnic differences. We examined the ethnic differences (Indian, Malay and Chinese) in IMCL in Singaporean children and the genetic risk variant(s) associated with these differences.Methods
The study population comprised 281 children (4.5 years old) from the ‘Growing Up in Singapore Towards healthy Outcomes’ (GUSTO) birth cohort [6]. All MR scans were performed without sedation on a Siemens Magnetom Skyra 3T scanner. Axial T1-weighted TSE images were acquired for voxel localization. Point-resolved spectroscopy (PRESS) scans were performed on a 1×1×1 cm3 voxel placed in the soleus muscle with the following parameters: TR=2000ms, TE =33ms, Averages = 24. The muscle spectra were quantified using LCModel. The IMCL levels were quantified by expressing the area of the IMCL methylene peak as a percentage of the area of the water peak from a water-unsuppressed scan. T2 correction of the IMCL and water peaks was performed using T2 values reported in literature [5]. Umbilical cord DNA samples of all the pediatric subjects were genotyped using Illumina Omniexpress + exome array covering ~1 million SNPs. For quality control, SNPs with call rates < 95%, MAF < 5%, or departed from the requisite assumptions of Hardy-Weinberg Equilibrium (HWE) were excluded. Since the sample size was smaller than standard for GWAS studies, both linear regression models and elastic net analyses were performed to identify the SNPs associated with IMCL.Results
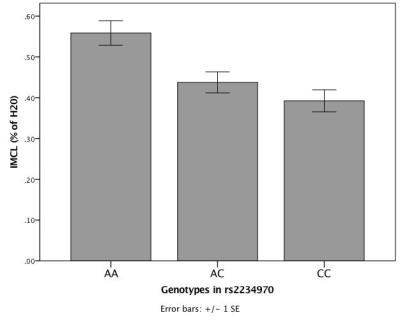
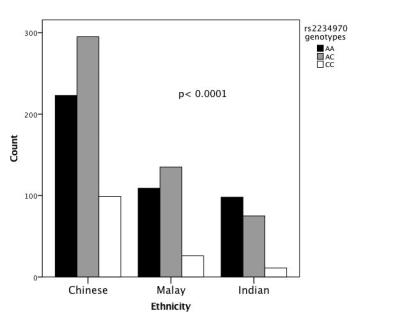
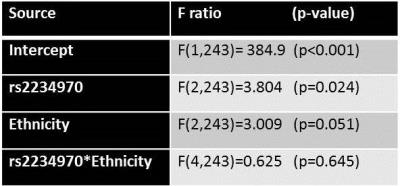
IMCL at 4.5 years differed significantly among the three ethnic groups with Indians having the highest IMCL (Fig. 1). GWAS analyses linked to IMCL identified a missense mutation (rs2234970; position 1160, M→L, P=3.38E-05) in the stearoyl-CoA desaturase 1 (SCD1) gene. Examining the SCD1 locus more closely, identified ‘A’ to be the risk allele associated with higher IMCL (Fig 2). An extended analysis of the ethnic distribution of rs2234970 genotypes in the entire GUSTO cohort (n=1071) revealed that Indian children carried two copies of the ‘A’ risk allele (Fig. 3) more frequently, than Chinese (OR=2.1, 95% CI (1.5-2.9)) or Malay (OR=1.7, 95%CI (1.2-2.5)) children. To study if the non-genetic component of ethnicity had an independent effect on IMCL, a 2-way ANOVA test was conducted with ethnicity and rs2234970 genotypes as factors. Only the main effect of the rs2234970 genotype was statistically significant (Table 1).Discussion and Conclusion
The higher accumulation of IMCL in Indian children, relative to Malay and Chinese children is in line with the trends observed in Asian adults [4]. This indicates that differential IMCL accumulation across ethnic groups can occur within 5 years of birth. The genome-wide association study suggests that the SCD1 locus, which codes for a lipid desaturase, may account for lipid accumulation within the skeletal muscle. This gene is also linked with obesity and insulin resistance in adults [7]. It is unclear whether the SCD1 locus causes both IMCL accumulation and insulin resistance, or if IMCL mediates the effect of SCD1 on insulin resistance. Indians have a higher frequency of the SCD1 risk allele, and the ethnic differences in IMCL accumulation between Indian, Malays and Chinese may at least be partly mediated by the rs2234970 genotype.Acknowledgements
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore.References
[1] DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009 Nov;32 Suppl 2:S157-63
[2] Guo Z, Intramyocellular lipids: maker vs. marker of insulin resistance. Med Hypotheses. 2008;70(3):625-9.
[3] Mellisa A Ashley, et al. Familial, Anthropometric, and Metabolic Associations of Intramyocellular Lipid Levels in Prepubertal Males. Pediatric Research (2002) 51, 81–86;
[4] Chin Meng Khoo et al. Body Fat Partitioning Does Not Explain the Interethnic Variation in Insulin Sensitivity Among Asian Ethnicity: The Singapore Adults Metabolism Study. Diabetes March 2014 vol. 63 no. 3 1093-1102.
[5] Alexandra Kautzky-Willer et al. Increased Intramyocellular Lipid Concentration Identifies Impaired Glucose Metabolism in Women With Previous Gestational Diabetes. Diabetes February 2003 vol. 52 no. 2 244-251.
[6] Soh SE et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. International journal of epidemiology 2014, 43:1401-1409.
[7] Sampath H, Ntambi JM. The role of stearoyl-CoA desaturase in obesity, insulin resistance, and inflammation. Ann N Y Acad Sci. 2011 Dec;1243:47-53.