3427
Sex and ethnic differences in abdominal fat partitioning and adipose tissue hydration in 4.5-year-old Asian children1Singapore Institute for Clinical Sciences, A*STAR, Singapore, 2Department of Obstetrics & Gynaecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 3Singapore BioImaging Consortium, A*STAR, Singapore, 4Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 5Department of Paediatric Endocrinology, KK Women’s and Children’s Hospital, Singapore, 6Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, 7MRC Lifecourse Epidemiology Unit & NIHR Southampton Biomedical Research Centre, University of Southampton & University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom, 8Clinical Nutrition Research Centre, Singapore Institute for Clinical Sciences, A*STAR, Singapore, 9Department of Endocrinology, Tan Tock Seng Hospital, Singapore, 10Department of Paediatrics, Faculty of Medicine, McGill University, Montreal, Canada, 11Department of Epidemiology, Biostatistics and Occupational Health, Faculty of Medicine, McGill University, Canada, 12Liggins Institute, University of Auckland, Auckland, New Zealand, 13Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital, Singapore
Synopsis
In this study, we used MR-based estimation of abdominal fat distribution and the degree of adipocyte hypertrophy to study sex and ethnic differences in 4.5-year-old Asian children. Our results show sexual dimorphism in abdominal fat distribution in preschool children. Girls had higher subcutaneous fat depot volumes and lower adipose tissue hydration than boys. We also found that at 4.5 years, both deep and superficial subcutaneous fat volumes in Indian children were higher, while the ethnic difference in internal fat was non-significant. These differences may help explain why Indians are more susceptible to metabolic and cardiovascular diseases.
Introduction
The study of childhood growth and adiposity is important for understanding the developmental origins of cardio-metabolic diseases. Studies have shown that sex and ethnic differences in abdominal fat distribution manifest very early in life [1,2]. Boys tend to accumulate more internal adipose tissue (IAT) while girls accumulate fat in the subcutaneous adipose tissue (SAT) [3-5]. Some ethnic groups also differ in their abdominal fat distribution [2,6,7]. Early identification of these differences may provide insights into predisposition to increased cardiovascular and metabolic diseases in later life. We have previously shown that the adipose tissue hydration is related to its morphological status [10]. Expansion of adipose tissue occurs through a combination of hyperplasia and hypertrophy. Lower relative water content (or conversely higher relative lipid content) is reflective of increased presence of large lipid filled adipocytes [10]. In this study, we evaluated the effect of ethnicity and gender on abdominal fat distribution and hydration in 4.5-year-old Asian children.Methods
We studied 316 subjects (158 Chinese, 94 Malay and 64 Indian; 150 boys and 166 girls) aged 4.5 years participating in the Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort [8]. Sum of skinfolds at four sites (biceps, triceps, subscapular and suprailiac) was used as a measure of overall adiposity. The subjects underwent MRI of the abdomen without sedation on the Siemens Skyra 3T MR scanner with Syngo VE 11A software. Sixty axial slices with 5-mm slice thickness and in-plane resolution of 0.94×0.94 mm were acquired using water-suppressed HASTE sequence (TR=1000ms, TE=95ms) and body matrix coil. A fully-automated graph theoretic segmentation algorithm [9] was used to segment and quantify the SAT and IAT depots between the liver dome and upper sacrum. The output image was then edited manually to remove bowel and other misclassified structures. The deep (DSAT) and superficial (SSAT) subcutaneous adipose tissue depots were segmented manually. The volume-localized 1H-MR spectrum of DSAT was obtained from a 1×1×1cm3 voxel at the level of the L5 lumbar vertebra using PRESS sequence (TR=2000ms, TE=30ms, 8 avg). The resonances were fitted and quantified using an in-house Matlab program. Adipose tissue hydration was assessed using the hydrolipidic ratio (HLR), defined as water/(water+fat).Results
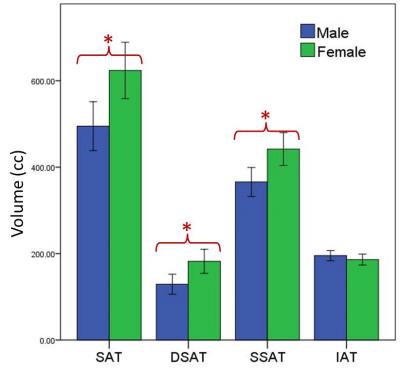
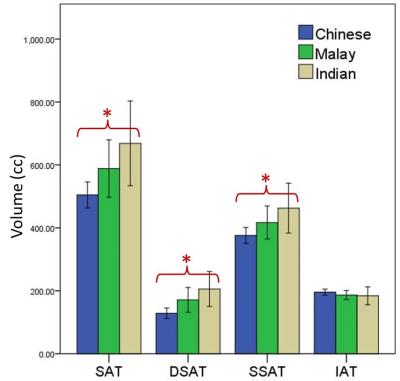
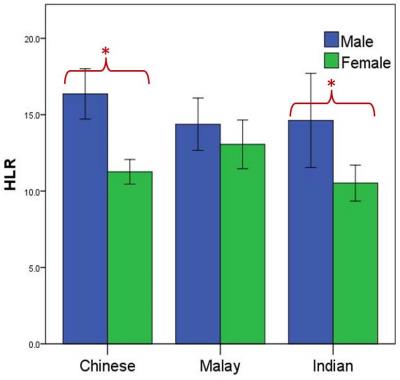
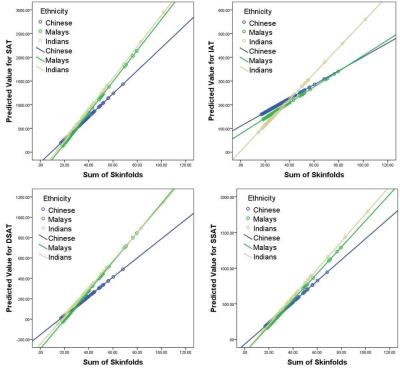
Figures 1 and 2 show the differences in abdominal fat distribution stratified by sex and ethnicity. We found that girls had significantly higher subcutaneous fat (total SAT, DSAT and SSAT) than boys. IAT was slightly higher in boys, but the difference was not statistically significant. The DSAT HLR was higher in boys than in girls (Figure 3). Among the ethnic groups, Indian children had the highest amount of subcutaneous fat (total SAT, DSAT and SSAT), followed by Malay and Chinese children. IAT and adipose tissue HLR were similar among the ethnic groups. We also tested for an ethnicity×sex interaction and found that sex modifies the association between ethnicity and DSAT HLR, but not the adipose depot volumes. We also found that ethnicity modifies the association between all the adipose depot volumes and overall adiposity, as assessed by the sum of skinfolds (Figure 4).Discussion and Conclusion
Our results show sexual dimorphism in abdominal fat distribution in preschool children. Girls had higher DSAT and SSAT volumes and lower adipose tissue HLR than boys. The DSAT and IAT depots have been associated with metabolic abnormalities. Our previous study reported that Indian and Malay neonates have a larger DSAT volume than Chinese neonates, without differences in SSAT and IAT volumes [2]. In this study we found that at 4.5 years, both DSAT and SSAT volumes in Indian children were higher, while the ethnic difference in IAT volume continued to be non-significant.
We also found that sex modifies the association between adipose tissue HLR and ethnicity, which may explain the absence of ethnic differences in HLR when the sexes were pooled. Among boys, the ethnic trends in DSAT volumes and HLR were in the opposite direction. Despite Chinese girls having a lower DSAT volume than Malay girls, they had a lower HLR (or increased lipid content), which is suggestive of increased presence of large adipocytes. This highlights the importance of measuring both fat volumes as well as fat quality.
With increasing overall adiposity (sum of skinfolds), Chinese had the lowest tendency to accumulate fat in all abdominal depots. Both Indians and Malays tended to accumulate DSAT and SSAT at similar rates, while Indians had the highest tendency to accumulate IAT. These differences may have long-term implications and the increased tendency to accumulate fat in pathogenic abdominal depots may help explain why Indians are more susceptible to metabolic and cardiovascular diseases.
Acknowledgements
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore.References
1. Modi N et al. Whole body magnetic resonance imaging of healthy newborn infants demonstrates increased central adiposity in Asian Indians. Pediatric research 2009, 1(65):584-7.
2. Tint MT et al. Abdominal adipose tissue compartments vary with ethnicity in Asian neonates: Growing Up in Singapore Toward Healthy Outcomes birth cohort study. The American journal of clinical nutrition 2016, 103(5):1311-7.
3. Karlsson AK et al. Measurements of total and regional body composition in preschool children: a comparison of MRI, DXA, and anthropometric data. Obesity 2013, 21(5):1018-24.
4. Staiano AE et al. Ethnic and sex differences in body fat and visceral and subcutaneous adiposity in children and adolescents. International journal of obesity 2012, 36(10):1261-9.
5. Kuk JL et al. Waist circumference and abdominal adipose tissue distribution: influence of age and sex. The American journal of clinical nutrition 2005, 81(6):1330-4.
6. Lear SA et al. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). The American journal of clinical nutrition 2007, 86(2):353-9.
7. Khoo CM et al. Body fat partitioning does not explain the interethnic variation in insulin sensitivity among Asian ethnicity: the Singapore adults metabolism study. Diabetes 2014, 63(3):1093-102.
8. Navin M et al. Adipose tissue hydration as a potential non-invasive marker for adipose tissue hypertrophy. Annual Meeting of the International Society for Magnetic Resonance in Medicine (ISMRM) 2015, p.0840.
9. Soh SE et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. International journal of epidemiology 2014, 43:1401-1409.
10. Sadananthan SA et al. Automated segmentation of visceral and subcutaneous (deep and superficial) adipose tissues in normal and overweight men. Journal of magnetic resonance imaging 2015, 41(4):924-34.
Figures