3364
Longitudinal MR Imaging Study of Standard Diffusion-Weighted Imaging and NODDI in ischemic Stroke: Evolution of NODDI metrics and Correlation with Clinical Outcome1Shaanxi Provincial People`s Hospital, Xi’an, People's Republic of China, 2Clinical science, Philips Healthcare China
Synopsis
To observe the microstructural longitudinal alterations in neural tissues after ischemic stroke and assess the correlation with clinical outcome and NODDI metrics. 18 subjects were enrolled. Intra-cellular volume fraction(Vic) and orientation dispersion index(OD) exhibited positive correlations with NIHSS scores of patients at day 30. The correlation of the susceptibility with the NODDI metrics and prognosis is higher than the ADC values with it. NODDI may provide a more promising and reliable methods for microstructural reorganization follow-up stroke than other measures previously used in studies of stroke recovery.
Introduction
Neurite orientation dispersion and density imaging (NODDI) is technique for an in vivo measure of the microstructural complexity of dendrites and axons complexity on clinical MRI scanners, which offers information complimentary to standard diffusion metrics and may potentially be a more sensitive biomarker for probing pathophysiological changes in stroke. At present, DWI is the most reliable neuroimaging technique for ischemic stroke assessment, however, ADC velues will gradually pseudo-normalized for 4-14 days after stroke onset, becoming normal or high in the subacute and chronic stages. The purpose of this study is to observe the microstructural complexity susceptibility dynamic changes in ischemic stroke from at day 1,day10 and day30 , elucidate the plausible biophysical mechanism and assess correlation with the clinical outcome and NODDI metrics.Methods
A total of 18 patients (age 65±7.8 years old) with ischemic stroke were involved with the approval of local IRB. Patients with a history of brain tumor or intracranial hemorrhages were excluded from study. All patients who underwent MRI and the National Institutes of Health Stroke Scale(NIHSS)at day 1,day10 and day30 after symptom onset were analyzed. MRI was performed on a 3.0T scanner (ingenia, Philips Medical Systems,The Netherlands),including routine sequences, DWI and NODDI. NODDI sequences were acquired with 3 b-values (0,1000 and 2000s/mm2) along 30 diffusion encoding directions with following parameters: TR/TE:2440/83ms, FOV=224x224mm2, acquisition matrix=112×112,image resolution=2.5×2.5x2.5mm2, acceleration factor=3, slice thickness=5 mm (no gap), acquisition time approximately 15 minutes. The post process was performed on NODDI Toolbox software and the noddi model ('WatsonSHStickTortIsoV_B0') implemented in MATLAB, the NODDI were calculated on a voxel-by-voxel basis. Parametric maps for orientation dispersion index(OD), intra-cellular volume fraction(vic), and isotropic (CSF) volume fraction(viso) were subsequently obtained. ROIs were manually identified by the hyperintensity on the diffusion-weighted images, ROIs were included the ischemic lesion with pixel values distinctly higher than the contralateral hemisphere, and any ambiguous pixels were not included. Percent change((ROIlesion-ROI normal)/ROInormal) of DWI and NODDI metrics from normal contralateral hemispheres to ischemic tissue was computed. The paired t-test was used to compare NODDI metrics and ADC values in normal and lesional tissue, we performed a one-way analysis of variance (ANOVA) on the percent change rADC,rOD, rvic and rviso in lesional tissue in every phases separately. we performed a Spearman correlation to test for the possible correlations between changes in the rADC, rOD, rvic and rviso at the first measures and the clinical outcome after 30 day.Results
Notice the distinct ischemic lesion signal heterogeneity on NODDI metrics that is not apparent on ADC maps,especically at day10 after stroke onset. OD and vic were higher in lesional tissue than contralateral normal zone, what is more, the percent change of OD value was from blow to high to below,vic was from high to below to below. The percent changes of viso were statistically decrease in the ischemic lesion, viso value was from blow to blow to high. OD and viso have significantly higher absolute percent change compared with complementary standard diffusion metrics at day 1 and day 10 after stroke (Table 1). We found that the percent changes in the rADC, rOD and rvic of the ischemic lesion the first 1 day after stroke were correlated with the NIHSS after 30 day in the stroke patients (Fig.2).Discussion
This longitudinal study confirms that NODDI indices are sensitive to pathological changes and microstructural complexity in stroke. Our results from NODDI indicate that ischemia causes a remarkable increase in neurite orientation dispersion and density, and the well-known decrease in ADC appears to be dominated by the change in the intra-axonal microenvironment of white matter. The change of NODDI indices that OD and vic values increase and viso reduce, may be consistent with lesional region of axonal swelling or beading of axons and dendrites as a result of osmotic imbalance. However, ADC value changes appear to be gradually pseudonormalized at day 10 after stroke (Fig.1), it was not significantly different change between the ischemic lesion and the contralateral normal hemisphere. We find that early changes in the rADC and NODDI metrics of the lesion may be useful for predicting the short-term clinical outcomes in stroke patients, these changes are be connected with severity of neurite lesion.
Conclusion
It suggested that NODDI may provide sensible neurite density and orientation dispersion estimates and more promising and reliable tool for assessment of complicated pathology of ischemic stroke, especially subacute stroke.Acknowledgements
The authors would like to thank Philips Healthcare for their technicalassistance.References
1. Zhang H, Schneider T, Wheeler-Kingshott CA, et al. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain.[J]. Neuroimage, 2012, 61(4):1000-1016.
2. Murphy TH, Li P, Betts K, et al. Two-photon imaging of stroke onset in vivo reveals that NMDA-receptor independent ischemic depolarization is the major cause of rapid reversible damage to dendrites and spines.[J].Journal of Neuroscience, 2008, 28(7):1756-72.
3.Copen WA, Schwamm LH, González RG, et al. Ischemic stroke: effects of etiology and patient age on the time course of the core apparent diffusion coefficient[J].Radiology, 2001, 221(1):27-34.
Figures
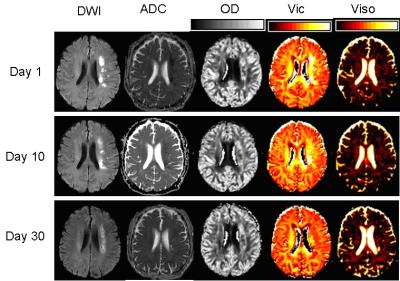
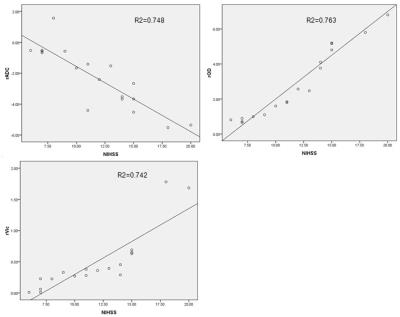

Table 1.ROI indicates region of interest; L:lesional; C:contralateral; PC:percent Change; ADC; OD:orientation dispersion index; vic:intra-cellular volume fraction; viso:isotropic (CSF) volume fraction.*Significant difference between the diffusion metrics in L and C. §△#Significant difference between the absolute percent change of conventional diffusion and NODDI metrics (ADC versus OD, ADC ersus viso, and ADC versus vic), OD and viso metrics (OD versus viso and OD versus vic ),vic and viso metrics (viso and vic), respectively. P<0.05 is considered statistically significant.