3323
Self-gated Non–Contrast-Enhanced Functional Lung (SENCEFUL) MRI for Evaluation of Endoscopic Lung Volume Reduction in Patients with Lung Emphysema1Department of Diagnostic and Interventional Radiology, University Hospital Würzburg, Würzburg, Germany
Synopsis
Purpose of the study was to assess the feasibility of SENCEFUL ventilation imaging for evaluation of therapy success after endoscopic lung volume reduction. Two patients with lung emphysema who underwent bronchial valve implantation were scanned before and after the procedure using SENCEFUL-MRI. Color-coded lung ventilation maps and quantitative ventilation values were pre- and postinterventionally compared. The first patient showed a ventilation defect corresponding to the location of the implanted valves with reduction of the quantitative ventilation. The second patient did not present such alterations and was later classified as non-responder to therapy. SENCEFUL-MRI detected clinically successful and non-successful outcomes correctly.
Purpose
The SENCEFUL (SElf-gated Non-Contrast-Enhanced FUnctional Lung imaging) approach is a recent development in functional lung MRI (1). This non-contrast-enhanced technique for the assessment of lung ventilation and perfusion is based on lung signal changes during the respiratory and cardiac cycle, which can be transformed in color-coded functional lung maps allowing for a spatially resolved assessment of lung function. Its feasibility for quantitative ventilation imaging in patients with cystic fibrosis and for detection of pulmonary embolism has recently been demonstrated (2,3).
Endoscopic lung volume reduction by bronchial valve implantation is a rather novel therapeutic approach for patients with severe emphysema. If successful, the treated lung segment with impaired gas exchange is no longer ventilated and the inspiratory air stream is redirected to less impaired lung segments resulting in improvement of clinical symptoms. Purpose of the present study was to assess the feasibility of SENCEFUL ventilation imaging for evaluation of therapy success in first patients after bronchial valve implantation.
Methods
Two patients who underwent bronchial valve implantation were examined using the SENCEFUL approach on a 3T scanner (Magnetom Skyra, Siemens Healthcare, Germany) equipped with a 32-channel body coil array. SENCEFUL is based on a 2D fast low-angle shot (FLASH) sequence with quasi-random sampling. By acquiring four additional data points without gradient-encoding (i.e. the center of k-space or direct current (DC) signal), the technique allows for cardiac and respiratory self-navigation by retrospectively segmenting each phase-encoding step to its position in the respiratory and cardiac cycle. Resulting ventilation measurements were quantified as proposed by Zapke et al. (4), providing quantification in ml gas exchange per ml lung volume (ml/ml). Quantitative lung ventilation maps were reconstructed and ventilation values were determined. Further details of data acquisition and image reconstruction have been described before (1).
In a 66 year-old female patient with chronic obstructive pulmonary disease (COPD) three bronchial valves were implanted in segmental bronchi of the left upper lobe and SENCEFUL-MRI was performed before and six days after the procedure. Five bronchial valves were implanted to the right upper lobe in a 58 year-old male subject with COPD and imaging was performed before and two days after valve implantation. The reconstructed color-coded lung ventilation maps and the quantitative ventilation values were intra- and interindividually compared.
Results
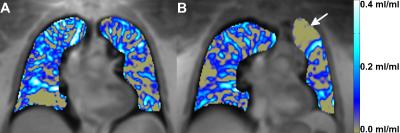
In the first patient the color-coded ventilation maps showed a ventilation defect in the left upper lung corresponding to the location of the implanted valves (Figure1). Follow-up chest x-rays confirmed development of an atelectasis in this area. Quantitative ventilation of the treated left upper lung decreased from 0.10 ml/ml before bronchial valve implantation to 0.01 ml/ml after the procedure whereas the ventilation remained constant in the right lung. Clinical assessment three months later showed improvement of symptoms with less dyspnea.
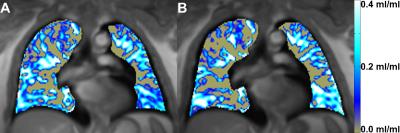
In the second patient the ventilation maps showed a small decline in ventilation in the peripheral right upper lung at the best (pre, 0.12 ml/ml; post, 0.10 ml/ml, Figure2). Neither follow-up chest x-rays nor morphological imaging during the MRI scan indicated the development of an atelectasis of the treated area. As valve implantation had not led to an improvement of symptoms most likely due to collateral ventilation, the clinical outcome was not satisfying, leading to the assumption of therapy failure with consecutive valve explantation three months later.
Discussion
SENCEFUL-MRI has been shown to detect and visualize ventilation and changes thereof with high spatial resolution. Both clinically successful and non-successful outcomes of bronchial valve implantation were detected correctly. Additionally contained morphologic information allows for detection of atelectasis with no need for dedicated diagnostic sequences or plain radiographs. Image comparison prior to and after intervention is possible not only by subjective judging of lung ventilation maps but also by objective quantification of ventilation in ml gas exchange per ml lung volume. The two presented cases indicate that response to valve implantation and success thereof can be gauged very early as SENCEFUL-MRI after two and six days post intervention, respectively, correctly anticipated clinical outcome as assessed up three months later. To date, indications for bronchial valve implantation remain under discussion (5). Providing comparable and quantifiable ventilation data with high spatial resolution, longitudinal SENCEFUL measurements in patient cohorts undergoing bronchial valve implantation could improve understanding of pathophysiological mechanisms and local implications of this procedure.Acknowledgements
No acknowledgement found.References
(1) Fischer A, Weick S, Ritter CO, Beer M, Wirth C, Hebestreit H, Jakob PM, Hahn D, Bley T, Köstler H. SElf-gated Non-Contrast-Enhanced FUnctional Lung imaging (SENCEFUL) using a quasi-random fast low-angle shot (FLASH) sequence and proton MRI. NMR Biomed. 2014 Aug;27(8):907-17.
(2) Veldhoen S, Weng AM, Knapp J, Kunz AS, Stäb D, Wirth C, Segerer F, Hebestreit H, Malzahn U, Köstler H, Bley TA. Self-gated Non-Contrast-enhanced Functional Lung MR Imaging for Quantitative Ventilation Assessment in Patients with Cystic Fibrosis. Radiology. 2016 Oct 6:160355. [Epub ahead of print]
(3) Kestler C, Weng AM, Kunz AS, Laubmeier M, Wirth C, Köstler H, Bley TA, Veldhoen S. Acute Pulmonary Artery Embolism Detected by Noncontrast Functional Lung Magnetic Resonance Imaging. Circ Cardiovasc Imaging. 2016 Feb;9(2):e004141.
(4) Zapke M, Topf HG, Zenker M, Kuth R, Deimling M, Kreisler P, Rauh M, Chefd'hotel C, Geiger B, Rupprecht T. Magnetic resonance lung function--a breakthrough for lung imaging and functional assessment? A phantom study and clinical trial. Respir Res. 2006 Aug 6;7:106.
(5) Kemp SV, Shah PL. An update on bronchoscopic treatments for chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2016 May;22(3):265-70.
Figures