3317
Self-gated ultra-short echo time lung MRI for quantitative ventilation assessment1Department of Diagnostic and Interventional Radiology, University Hospital Wurzburg, Wurzburg, Germany
Synopsis
Self-gated Non-Contrast-enhanced Functional Lung MRI (SENCEFUL) is a technique based on a FLASH sequence that can assess ventilation and perfusion in free-breathing without the use of contrast agents. However, SENCEFUL suffers from the fast T2-induced signal decay in the lung parenchyma and offers no real 3D coverage. Thus, this work presents the use of a 3D ultra-short echo time (UTE) sequence in SENCEFUL MRI for the generation of ventilation-weighted maps.
Purpose
The combination of Fourier decomposition MRI with direct current (DC; signal at k=0) gating enabled the assessment of functional and morphological information of the lung in free-breathing [1,2].Based on this concept, Self-gated Non-Contrast-enhanced Functional Lung MR Imaging (SENCEFUL) is a robust technique that can assess ventilation and perfusion in free-breathing without the use of contrast agents, hyperbolized gases or radiation [1,3]. However, SENCEFUL uses a 2D low-angle shot (FLASH) sequence, which suffers from the fast signal decay in the lung parenchyma and offers no real 3D coverage. Aiming to improve the signal to noise ratio and to reduce the T2-induced signal decay, this work introduces the use of an ultra-short echo time (UTE) sequence in SENCEFUL MRI.Methods
A UTE pulse sequence, consisting of a nonselective RF pulse excitation followed by a 3D koosh ball acquisition, was developed. Thus, the first samples of the ADC in the k-space center serve as DC-gating, which can be evaluated for each coil. In order to make sure that the center of the k-space was acquired, a delay of 10μs between the start of the ADC and the read-out gradients was applied. The UTE SENCEFUL measurements were performed on a 3 T MR system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) equipped with a 32-channel coil-array in a healthy volunteer during free-breathing, according to the following parameters: TE = 0.07 ms; TR = 6.0 ms; flip angle = 2°; FOV = 300x300mm; number of spokes = 300000 and matrix size = 128x128. Afterwards, the DC-signal from each coil was plotted to identify the coil best suited for respiratory data binning. Seven different breathing states were segmented, representing one breathing cycle from expiration to inspiration. Each state contained at least 30000 spokes, with a sampling density that is 58% of the Nyquist sampling rate. Iterative SENSE [4] was then used for a separate reconstruction of each data set, leading to a time series of one breathing cycle. For quantitative assessment of the ventilation three coronal slices were averaged to achieve a better signal-to-noise ratio. The calculation of the quantitative ventilation map was performed as proposed earlier by applying a Fourier transform along the temporal dimension [1,2]. Finally, the ventilation for all sectors of the lung was quantified [5].Results
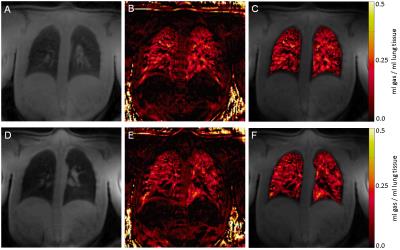
Figure 1 shows three orthogonal slices for four different reconstructed breathing states, where the breathing motion and lung morphology of the healthy volunteer can be clearly contemplated. The improved signal of the UTE sequence in the lungs allows to clearly delineate the lung parenchyma, air ways and blood vessels. Figure 2 presents two quantitative ventilation maps reconstructed from the SENCEFUL UTE MRI measurement of the healthy volunteer shown in Figure 1. The quantitative values (ml of gas per ml of lung tissue) calculated for the left and right lungs for the two different slices shown in Figure 2 were: left lung = 0.12 ± 0.07 and 0.10 ± 0.08 ml/ml; right lung = 0.10 ± 0.08 and 0.10 ± 0.07 ml/ml. This corresponds to values previously published using SENCEFUL with a FLASH sequence: 0.12 ml/ml for the left lung and 0.11 ml/ml for the right lung [3].Discussion
Pulmonary ventilation could be successfully assessed using an UTE sequence for SENCEFUL MRI. When compared to the use of FLASH, UTE has provided a better representation of the lung morphology, a 3D reconstruction of the breathing cycle and the possibility of assessing the ventilation for multiples slices with only one measurement. Also, SENCEFUL using FLASH has previously presented limitations related to the slice thickness, which have led to pseudo-ventilation effects [3]. Due to its higher signal intensity, UTE could offer a smaller slice thickness compared to the 2D FLASH approach. On the other hand, our 3D UTE technique was not able to detect perfusion-related signal variations in the lung because it is not possible to use the inflow effect of unsaturated spins in this 3D application. However, there are 2D UTE approaches that might overcome this drawback.Acknowledgements
No acknowledgement found.References
1. Fischer A, Weick S, Ritter C. O, et al. SElf-gated Non-Contrast-Enhanced FUnctional Lung imaging (SENCEFUL) using a quasi-random fast low-angle shot (FLASH) sequence and proton MRI. NMR in Biomedicine. 2014;27(8), 907–17.
2. Bauman G, Puderbach M, Deimling M, et al. Non-contrast-enhanced perfusion and ventilation assessment of the human lung by means of fourier decomposition in proton MRI. Magnetic Resonance in Medicine. 2009;62(3), 656–64.
3. Veldhoen S, Weng A M, Knapp J, et al. Self-gated Non-Contrast-enhanced Functional Lung MR Imaging for Quantitative Ventilation Assessment in Patients with Cystic Fibrosis. Radiology. 2016; 160355.
4. Pruessmann KP, Weiger M, Bornert P, Boesiger P. Advances in sensitivity encoding with arbitrary k-space trajectories. Magn Reson Med. 2001 Oct;46(4):638-51
5. Zapke M, Topf HG, Zenker M, et al. Magnetic resonance lung function - a breakthrough for lung imaging and functional assessment? A phantom study and clinical trial. Respiratory Research. 2006;7:106.
Figures