3314
Diagnosing Lung Nodules on various MRI Imaging: comparison of T1-Weighted-3D VIBE-dixon sequence and T1-weighted 3D star vibe sequence1The first affiliated hosptial of Shaanxi traditional chinese medical university, Xian Yang, People's Republic of China
Synopsis
T1-weighted 3D Star VIBE sequence obtaining scan under free breathing can provide high-resolution imaging. Therefore, our study was to assess the accuracy of various MRI sequences for the diagnosis of pulmonary nodules and to estimate the ability of MRI for display the morphology of pulmonary nodules. We concluded that T1-weighted 3D Star VIBE sequence allow for identification of patients with pulmonary nodules with high detection rate. It can also provide more information of nodules than routine T1-weighted 3D VIBE sequence dose.
PURPOSE
Magnetic resonance imaging (MRI) has been suggested in clinical application of lung lesion detection with multiple advantages including improved soft-tissue contrast and the reduced radiation exposure. In patients with lung nodules, it is extremely important to detect the presence of nodules and display their morphology correctly for enhancing treatment decision. The T1-weighted-3D VIBE-dixon sequence produced thinner image slices and a higher resolution than conventional MR sequences [1], so it is reported to be used in lung nodules detection [2.3]. However, there is still significant number of false positive diagnoses. T1-weighted 3D Star VIBE sequence obtaining scan under free breathing can also provide high-resolution imaging. Therefore, our study was to assess the accuracy of various MRI sequences for the diagnosis of pulmonary nodules and to estimate the ability of MRI for display the morphology of pulmonary nodules.
METHODS AND MATERIALS
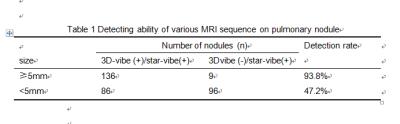
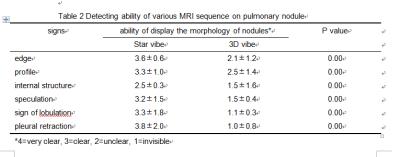
Ten patients with 327 nodules diagnosed by CT underwent lung MRI for follow-up observation was enrolled in this study. Exclusion criteria were contraindications to MR imaging such as pacemakers, metal implants and younger than 18 years. The MRI protocol ((MAGNETOM 3.0T SKYRA MR scanner, Siemens healthcare, Erlangen, Germany)) included a T2-weighted-tirm HASTE sequence (TE/TR:106 ms/∞, slice thickness 5mm), T1-weighted-3D VIBE-dixon sequence (TE1、TE2/TR:1.29、2.52/3.97 ms, slice thickness 3mm) and a T1-weighted 3D Star VIBE sequence(TE/TR:1.39/2.79,slice thickness 1.2mm). 3D VIBE and Star VIBE data were analyzed independently by two radiologists. Each MRI sequence was evaluated for the detection of pulmonary nodules and the ability of display the morphology of pulmonary nodules (edge, profile, and internal structure, speculation, sign of lobulation, pleural retraction). The ability of display the morphology of pulmonary nodules was evaluated by 4 point scale (4=very clear, 3=clear, 2=unclear, 1=invisible).RESULTS
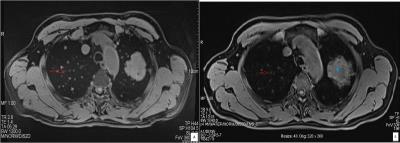
A total of 327 nodules were detected on Star VIBE sequence image, while only 222 nodules were detected on 3D vibe sequence image. The overall detection rate of 3D vibe was 67.9% when served the Star VIBE as a reference sequence. According to the nodules size: the detection rate was 93.8% for nodules≥5mm, and the detection rate was 47.2% for nodules<5mm (table1,figure1). The ability of display morphology of pulmonary nodules was evaluated in 13 nodules (≥5mm) detected in both 3D vibe image and Star VIBE image. The ability was significantly difference between Star VIBE image and 3D vibe image in each signs (p=0.000, edge: 3.6±0.6 VS 2.1±1.2; profile: 3.3±1.0 VS 2.5±1.4;internal structure:2.5±0.3 VS 1.5±1.6;speculation 3.2±1.5 VS 1.5±0.4;sign of lobulation 3.3±1.8 VS 1.1±0.3; pleural retraction 3.8±2.0 VS 1.0±0.8,table2).Conclusion
T1-weighted 3D Star VIBE sequence allow for identification of patients with pulmonary nodules with high detection rate. It can also provide more information of nodules than routine T1-weighted 3D VIBE sequence dose.Acknowledgements
No acknowledgement found.References
[1] Ang EC, Robertson AF, Malara FA, O'Shea T, Roebert JK, Schneider ME, Rotstein AH. Diagnostic accuracy of 3-T magnetic resonance imaging with 3D T1 VIBE versus computer tomography in pars stress fracture of the lumbar spine. Skeletal Radiol. 2016; 45(11):1533-40.
[2] Schaarschmidt B, Buchbender C, Gomez B, Rubbert C, Hild F, Köhler J, et al. Thoracic staging of non-small-cell lung cancer using integrated (18)F-FDG PET/MR imaging: diagnostic value of different MR sequences. Eur J Nucl Med Mol Imaging. 2015; 42(8):1257-67.
[3] Chandarana H1, Block KT, Winfeld MJ, Lala SV, Mazori D, Giuffrida E, Babb JS, Milla SS. Free-breathing contrast-enhanced T1-weighted gradient-echo imaging with radial k-space sampling for paediatric abdominopelvic MRI. Eur Radiol. 2014; 24(2):320-6
Figures