3308
Optimized 3D ultrashort echo-time lung imaging of young children without sedation1University of Rochester, Rochester, NY, United States, 2Indiana University, Indianapolis, IN, United States, 3Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
Synopsis
Our purpose was to develop an optimized study design for 3D ultrashort TE lung imaging of young children without sedation. Eight preterm born subjects all at age 4 were recruited. Siemens work-in-progress PETRA_D sequence was used with respiratory triggering. Repeated short scans were acquired to reduce motion artifacts. Various techniques, including video watching, practicing lying still at home and gift incentive, were employed to help achieve subject compliance. Five subjects were scanned successfully. The images revealed abnormalities including peribronchial thickening, pneumatocele and atelectasis. Our study design allows the monitoring of lung development and evaluation of lung diseases in young children.
Purpose
Interest in ultrashort echo-time MRI has recently been expanding for lung imaging 1-2. It is particularly advantageous to children because of its non-ionizing nature. However, most studies have been conducted on adults, school-age pediatrics or swaddled neonates 3-5. However, for younger children, there are additional study design considerations to limit scan times and help achieve subject compliance. Our objective is to develop and evaluate a study design for 3D ultrashort TE lung imaging of young children below 5 years of age without sedation.Methods
The study was conducted on a 3T Siemens TRIO system. Eight preterm born subjects (5 male, 3 female, 4.0 to 4.9 years old) were recruited. Ultrashort TE lung images were acquired using PETRA_D 6 obtained from Siemens HealthCare as a work-in-progress sequence. At study scheduling (typically 3 weeks ahead), the contact parent was asked to have the subject practice lying still at home. At the study session, a child life specialist experienced in working with children undergoing MRI exams showed the subjects a model MR scanner and played a recording of MRI sounds. The subjects were promised a toy that they could select later as an incentive for lying still. Moreover, the subjects chose a cartoon movie to watch inside the scanner. Since the head coil with a viewing mirror interfered with the placement of the body matrix coil, it could not be used for video watching and a custom plastic mirror setup was constructed for this purpose (Fig. 1). Audio was transmitted through a pneumatic headphone. Axial PETRA_D images were acquired with FOV 30cm, TR 2.1ms, TE 0.09ms, matrix size 224 to 256, 3D isotropic resolution 1.12 to 1.34 mm and 60,000 radial views. To optimize SNR, the Ernst angle of 30 was used. Respiratory triggering was applied with a respiratory bellow (30% threshold at end expiration). The scan time was about 4 mins. To prevent aliasing image artifact, only the superior section of the body matrix coil and one section of the spine coil were selected. The scan was repeated once or twice to test for variation in image quality. The images were evaluated by a radiologist for diagnostic quality and lung abnormalities.Results
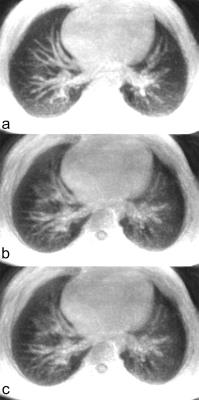
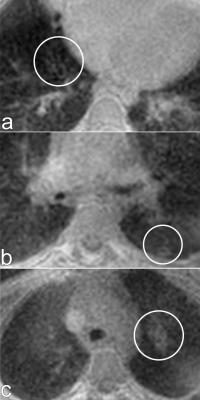
Five subjects were scanned successfully providing readable images. The other three subjects were reluctant to enter the scanner. For each scanned subject, the first scan had the best image quality with the least motion blurring (Fig. 2), implying compliance may decrease with study duration. Lung abnormalities observed include peribronchial thickening, pneumatocele and atelectasis (Fig. 3).Discussion
With optimized study design, useful ultrashort TE lung images could be obtained from young children under 5 without sedation. All 5 scanned subjects appeared calm and focused on the movie during the scans. Sedation-free scanning avoids the need of an anesthesiologist, prevents confounding factor of dependent atelectasis and is more likely to be accepted by parents of potential research subjects.
Though a more typical radial UTE sequence was also available to us 5, PETRA_D was used in this study because it is compatible with respiratory gating and is quieter 6, both features are important for imaging small children.
Only the first subject went through the mock scanner to get accustomed to the MRI environment after a recommendation from the child life specialist that it might have been too much information in a short time. The outcome of this study appears to support this decision, which simplifies the protocol for other sites.
Since image quality can vary significantly among the different scans of a subject due to body motions, shorter and repeated scans as those used in this study appear more desirable as they have less chance to be affected by motion and allow the selection of the best scan to be used in lung evaluation.
Conclusion
We have developed an optimized study design for 3D ultrashort TE lung imaging of young children without sedation. This design allows the monitoring of lung development and evaluation of lung diseases during preschool. The techniques involved may also be applicable to older children.Acknowledgements
The authors would like to thank Siemens Healthcare for providing the PETRA_D sequence for this study. We would also like to thank Liz Werner for coordinating the study.References
1. Ma W, Sheikh K, Svenningsen S, et al. Ultra-short echo-time pulmonary MRI: evaluation and reproducibility in COPD subjects with and without bronchiectasis. J Magn Reson Imaging. 2015;41(5):1465-1474.
2. Lederlin M, Crémillieux Y. Three-dimensional assessment of lung tissue density using a clinical ultrashort echo time at 3 Tesla: a feasibility study in healthy subjects. J Magn Reson Imaging. 2014;40(4):839-847.
3. Gai ND, Malayeri A, Agarwal H, Evers R, Bluemke D. Evaluation of optimized breath-hold and free-breathing 3D ultrashort echo time contrast agent-free MRI of the human lung. J Magn Reson Imaging. 2016;43(5):1230-1238.
4. Hahn AD, Higano NS, Walkup LL, et al. Pulmonary MRI of neonates in the intensive care unit using 3D ultrashort echo time and a small footprint MRI system. J Magn Reson Imaging. 2016 [Epub ahead of print].
5. Kwok WE, Ren C, Pryhuber G, Chess M, Woods JC. High-resolution 3D ultra-short echo-time imaging of the lung in young children at 3T without sedation. In: Proceedings of ISMRM 24th Scientific Meeting and Exhibition, Singapore 2016, p1619.
6. Grodzki DM, Jakob PM, Heismann B. Ultrashort echo time imaging using pointwise encoding time reduction with radial acquisition (PETRA). Magn Reson Med. 2012;67(2):510-518.
Figures