3301
Does PROPELLER acquisition improve bladder imaging by substantially reducing motion artifacts?1Wright Center of Innovation in Biomedical Imaging, Department of Radiology, The Ohio State University, Columbus, OH, United States, 2Center for Biostatistics, The Ohio State University, Columbus, OH, United States
Synopsis
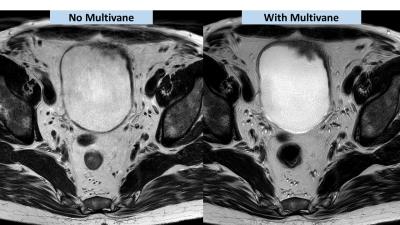
This study is to evaluate the clinical application of PROPELLER reconstruction technique to reduce breathing-induced motion artifacts in bladder imaging. High resolution T2W images were acquired with and without multivane (PROPELLER technique) in fourteen patient scans. Image quality was assessed by a radiologist in terms of motion artifacts and the visualization of tumor margins. Scores were given in the range of 1 to 4. The results showed that the application of multivane significantly improved both motion artifacts and tumor visualization (both P<0.001). In conclusion, PROPERLLER reconstruction is a robust technique to substantially reduce the artifacts caused by unavoidable breathing motion to provide the delineation of bladder tumors against surrounding tissues.
Purpose
This study is to evaluate the clinical utility for bladder imaging of applying a k-space sampling method that uses rotating strips of multiple phase-encoding lines, called Periodically Rotated Overlapping Parallel Lines with Enhanced Reconstruction (PROPELLER), to reduce the breathing-induced motion artifacts on bladder in morphologic T2-weighted (T2W) MRI at 3T MRI.Materials and Methods
Subjects
Within a multi-phasic clinical trial effort to enhance the imaging of bladder cancer for the improvement of the cancer diagnosis, the utility of PROPELLER was investigated. If motion was seen on T2W MR images, T2W-MRI with multivane, the Philips acronym of PROPELLER, was performed right after the first T2W. Fifteen bladder patient scans were included in this study performed on an 3T Ingenia CX.
MRI protocol
Both T2W MRI with and without multivane were performed with Turbo Spin Echo (TSE) sequence. The imaging parameters of T2W without multivane were TR/TE, 5480/91 ms; matrix, 100/140; in-plane FOV (AP/RL), 300/340 mm; slice thickness = 3.0 mm; slice gap = 0.3 mm; in-plane resolution, 0.5x0.5 (mm); number of slices = 45; number of signal average = 1; SENSE factor, 2; scan time, 285s. The parameters with multivane were TR/TE, 6278/125 ms; in-plane FOV (AP/RL), 300/300 mm; slice thickness = 3.0 mm; slice gap = 0.3 mm; in-plane resolution, 0.5x0.5 (mm); number of slices = 45; number of signal average = 1; SENSE factor, 3; scan time, 327s; Multivane factor was 360%.
Data analysis
A radiologist reviewed T2W data with and without multivane to assess the quality of images for diagnosis. Two assessment tasks were performed. Scores were given in the range of 1 to 4. Motion assessment: highest score of 4 was given when no motion was seen and images were clear; score of 3 when some (little) motion was seen.; score of 2 when significant motion was seen, but still acceptable; score of 1 when severe motion was seen and images were not assessable. Visualization assessment: highest score was given when all tumor margin was clearly visualized on on the bladder wall; score of 3 when tumor margins were still seen on the bladder wall; score of 2 when tumor was identified but its margin cannot be determined; score of 1 when tumor cannot be localized.
The image quality was compared between T2W with and without multivane (PROPELLER). P<0.05 was considered to be statistically significant.
Results
Motion induced artifacts were shown to be substantially reduced in all cases that applied the PROPELLER method during bladder imaging. Median scores based on motion were 2 without and 4 with multivane. As for tumor visualization, the application of multivane led to better delineation of the tumor margins and thus increased the diagnostic certainty of bladder cancer. The median scores for tumor visualization were 2.5 without and 4 with multivane. The statistical analysis showed that the application of multivane significantly (both P<0.001) improved both motion-induced artifacts and tumor visualization. At the same time, the spatial resolution, similar signal contrast, and comparable scan time were all maintained.Discussion
Imaging of the bladder is often severely affected by unavoidable breathing motion as the organ is close to the superficial abdominal fat. With similar coverage, scan time and image contrast, the application of this radial k-space sampling technique can significantly reduce motion-induced artifacts and provides high quality imaging of the morphology of the bladder as well as the pelvis.Conclusion
Motion artifacts suppressing k-space sampling improves clinical imaging and the diagnosis of bladder cancer as well as the quality of pelvic imaging overall. We have identified any drawbacks so that routine applications of this approach should be considered as the bladder wall and lesion can be overshadowed otherwise by motion-induced artifacts.Acknowledgements
This study is supported by Wright Center of Innovation in Biomedical Imaging development fund and ODSA TECH 13-060.References
1. Dietrich TJ, Ulbrich EJ, Zanetti M, Fucentese SF, Pfirrmann CW: PROPELLER technique to improve image quality of MRI of the shoulder. AJR American journal of roentgenology 2011, 197(6):W1093-1100.
2. Nguyen HT, Pohar KS, Jia G, Shah ZK, Mortazavi A, Zynger DL, Wei L, Clark D, Yang X, Knopp MV: Improving bladder cancer imaging using 3-T functional dynamic contrast-enhanced magnetic resonance imaging. Investigative radiology 2014, 49(6):390-395.
3. Pipe JG. Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 1999; 42:963-969.
Figures