3285
MR renography shows that serum-clearance methods overestimate GFR in patients with ascites1Department of Radiology and Imaging Sciences, University of Utah, Salt Lake City, UT, United States, 2Department of Radiology, Northwestern University, Chicago, IL, United States
Synopsis
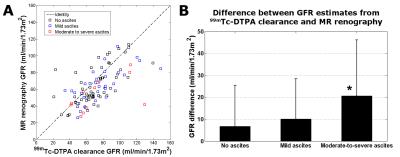
In this study, the impact of ascites on clearance-based GFR estimation was examined by comparing GFR estimates from 99mTc-DTPA clearance and MR renography in cirrhosis patients with varying degrees of ascites. 99mTc-DTPA clearance significantly overestimated GFR relative to MR renography in patients with moderate-to-severe ascites, likely because of extra-renal clearance of tracer into abdominal ascites fluid. Conversely, MR renography was unaffected by the presence of ascites because it tracked uptake and excretion of tracer specifically by the kidneys. This ascites-insensitivity makes MR renography a promising technique for GFR assessment in cirrhosis patients, a population with a high incidence of ascites.
Motivation
Renal dysfunction commonly afflicts those with liver cirrhosis,1 and the accurate assessment of renal function is therefore important for the clinical management of cirrhosis patients. Glomerular filtration rate (GFR) is the most widely reported metric of renal function, and is generally estimated by measuring the clearance of a tracer (such as 99mTc-DTPA) from the blood. This approach assumes that renal filtration is solely responsible for the clearance of tracer. When ascites is present, however, tracer may also exit the blood into ascites fluid in the peritoneal cavity, resulting in misleadingly high clearance of tracer and overestimation of GFR. Ascites commonly develops with cirrhosis, and it is therefore important to consider the impact of ascites on clearance-based GFR estimation techniques. MR renography2 is an alternative method for estimating GFR that repeatedly images the kidneys to record and analyze the uptake of MRI contrast agent by the glomeruli and its transit through the renal tissues. Since it directly examines the filtration of tracer by the kidneys, MR renography avoids the confounding effects of extra-renal clearance. In this study, the impact of ascites on clearance-based GFR estimation was examined by comparing GFR estimates from 99mTc-DTPA clearance and MR renography in cirrhosis patients with varying degrees of ascites.Methods
In this IRB-approved study, GFR was estimated from 104 cirrhosis patients (35 female, 69 male; ages 20-81) using both 99mTc-DTPA clearance and MR renography. Both techniques were performed on the same day following informed consent. For each patient, ascites was evaluated from MR images by an experienced reader and categorized as either: not present, mild, or moderate-to-severe. The difference in GFR estimates from the two techniques was compared between the three categories of ascites. We hypothesized that clearance-based GFR estimates would be significantly larger than those from MR renography in patients with ascites, as a result of extra-renal clearance of tracer into ascites fluid.
99mTc-DTPA clearance: 5 mCi of 99mTc-DTPA was injected intravenously, and urine samples were collected 150 and 240 minutes after injection. Peripheral venous blood samples were collected 60, 150, and 240 minutes after contrast injection. For each urine sample, GFR was estimated using the formula: GFR = U∙V/P, where U is the concentration of the tracer in the urine (counts/min/ml), V is the urine flow rate (ml/min), and P is the average concentration of tracer in the blood samples bracketing the urine sample.
MR renography2: All MR imaging was performed at either 1.5T or 3T (Avanto or TimTrio; Siemens). MR renography used a 2D single-shot gradient echo sequence with a preparatory nonselective saturation-recovery pulse: TR 526ms, TE 1.21ms, flip angle 16°, matrix 154×176, FOV 382×420mm. Following an intravenous bolus-injection of 4ml gadoteridol (Prohance; Bracco), dynamic images of the kidneys and abdominal aorta were repeatedly acquired for ~5 minutes. Contrast-enhancement curves from the kidneys and aorta were then analyzed with a tracer-kinetic model3 to extract GFR.
Ascites evaluation: Ascites was assessed from MR images acquired using a 3D T2-weighted fast spin echo sequence with fat saturation4: TR 4000ms, TE 123ms, matrix 256×256×46, FOV 400×400×220mm. On these images, ascites fluid appeared as bright signal adjacent to the liver. Ascites was graded as mild, moderate, or severe based on the degree of liver displacement caused by ascites fluid accumulation (Figure 1).
Results
Of the 104 patients in this study, 102 completed all examinations. Two patients did not produce sufficient urine for the 99mTc-DTPA clearance examination. Ascites was present in 43 of the 102 patients. Of these 43 ascites cases, 11 were categorized as moderate-to-severe. Figure 2 compares GFR measurements from 99mTc-DTPA clearance to those from MR renography. In the group with moderate-to-severe ascites, 99mTc-DTPA clearance overestimated GFR relative to MR renography by 20.7±25.4 ml/min/1.73m2, which was significantly higher (P=0.02) than the overestimation observed in patients with no ascites (6.8±18.6 ml/min/1.73m2). Clearance-based GFR overestimation in the group with mild ascites (10.1±18.2 ml/min/1.73m2) was also higher than in those with no ascites, but this increase was not statistically significant (P=0.21).Discussion
99mTc-DTPA clearance significantly overestimated GFR relative to MR renography in patients with moderate-to-severe ascites, i.e., with substantial accumulation of fluid in the abdomen. This result suggests that extra-renal clearance of tracer can cause significant overestimation of renal function when clearance-based estimation techniques are used. Conversely, MR renography is not affected by the presence of ascites because it tracks the uptake and excretion of tracer specifically by the kidneys. This ascites-insensitivity makes MR renography a promising technique for GFR assessment in cirrhosis patients, a population with a high incidence of ascites for whom renal function measurement is important.Acknowledgements
References
1. Mackelaite L, Alsauskas ZC, Ranganna K. Renal failure in patients with cirrhosis. Med Clin North Am 2009;93(4):855-869.
2. Vivier PH, Storey P, Rusinek H, et al. Kidney function: glomerular filtration rate measurement with MR renography in patients with cirrhosis. Radiology 2011;259(2):462-470.
3. Zhang JL, Rusinek H, Bokacheva L, et al. Functional assessment of the kidney from magnetic resonance and computed tomography renography: impulse retention approach to a multicompartment model. Magn Reson Med 2008;59(2):278-288.
4. Lauenstein TC, Sharma P, Hughes T, Heberlein K, Tudorascu D, Martin DR. Evaluation of optimized inversion-recovery fat-suppression techniques for T2-weighted abdominal MR imaging. J Magn Reson Imaging 2008;27(6):1448-1454.
Figures