3282
Transpedal MR-lymphangiography - A new imaging tool for pre-interventional planning of lymphatic interventions in patients with chylous effusions1Radiology, University Hospital Bonn, Bonn, Germany
Synopsis
Lymphatic interventions are increasingly performed for the treatment of chylous leakages. Pre-interventional evaluation of the central lymphatic system is important for adequate patient selection and planning of the interventional technique. We describe a new transpedal approach for MR-lymphangiography (tMRL) to evaluate the anatomy of central lymphatics including anatomical variations, as well as for detection of leakages and analysis of a potential interventional access site. Our results demonstrate that central lymphatic anatomy can be readily evaluated using tMRL in the majority of patients scheduled for lymphatic interventions. It is a well-tolerated, valuable diagnostic tool in the pre-interventional work-up of lymphatic interventions.
Purpose
Chylous leakages (especially chylothorax and chylascites) can occur after trauma / surgery, as consequence of various medical diseases or spontaneously, and have a considerable morbidity and mortality1. Interventional treatment options based on lymphangiography using iodized oil with subsequent cannulation and embolization of the thoracic duct (TD) are increasingly employed2-6. Conventional or intranodal lymphangiography provides dynamic high-resolution images of central lymphatics, but is time-consuming, invasive, delivers only 2-dimensional images and involves risks from the oily contrast agent. Pre-interventional evaluation of the central lymphatic system therefore is important for adequate patient selection and planning of the invertentional procedure. The aim of this study was to evaluate the clinical usefulness of transpedal MR-lymphangiography (tMRL) in the pre-interventional work-up for lymphatic interventions in patients with chylous effusions.Materials and Methods
tMRL was performed in 30 patients (m/f : 15/15, mean age 55 years) with chylous effusions scheduled for lymphatic intervention. Indications were: traumatic/iatrogenic chylothorax n=7, non-traumatic chylothorax n=9, traumatic/iatrogenic chylascites n=4, non-traumatic chylascites n=3, combined chylothorax/chylascites n=5, post-operative cervical fistula n=1 and recurrent neck swelling n=1.
Patients underwent tMRL on a 1.5T scanner (Philips Healthcare, Best, The Netherlands; Ingenia; gradient system: maximum amplitude of 45 mT/m, maximum slew rate of 200 T/m/s) with T1-weighted imaging employing a breath-hold mDIXON sequence after intradermal pedal injection of gadolinium contrast-medium (Gadobutrol 1.0 mmol/ml) under local anesthesia.
Contrast-enhanced images were evaluated regarding depiction of a leakage site, a possible access route for lymph vessel embolization and anatomical variations.
Results
Contrast injection was well tolerated in all patients without complications. Sedation was necessary in one case. In 25/30 patients (83.3%) enhancing central lymphatics were detectable (cause of failure: restlessness despite sedation n=1, lymphoma with lymphedema n=1, technical reasons n=3).
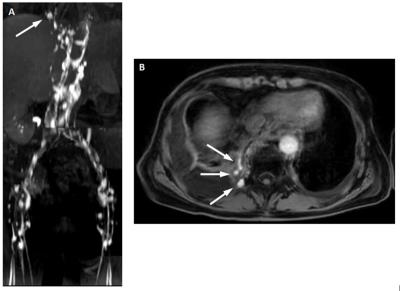
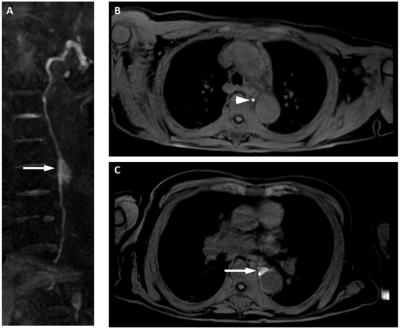
Leakage was identified in 17/25 technically success examinations (68%) (Figure 1, 2). In 6 patients with chylascites, contrast medium leaked intraabdominally and did therefore not reach the cisterna chyli. In the remaining 19 patients with thoracic or cervical pathologies a possible access site for thoracic-duct embolization was identified in 18/19 patients (cisterna chyli in 15/19, thoracic-duct (TD) in 18/19 [12 continuous, 6 discontinuous enhancement]). 6/18 patients had a single thoracic duct, 12/18 a duplicated thoracic duct. In one patient the duct terminated in the right venous angle.
Overall 25/30 tMRL-exams (83.3%) provided clinically useful information to guide lymphatic interventions.
Discussion
The results of our study demonstrate that tMRL can provide information on the anatomy of the central lymphatic system including a potential interventional access site in the majority of patients. Hereby, tMRL can influence the treatment strategy and facilitate the intervention itself.
The leakage site, however, could only be identified in 68 % of cases. This may in part be due to only intermittent lymphatic leakage and is in line with conventional lymphangiography - which is considered the gold standard for detection and characterization of lymphatic leakages - which also has a detection rate of 64-78 %7-9.
A dynamic MRL technique via sonography guided intranodal contrast injection during the MR-exam has recently been described10. It has so far only been performed under general anesthesia. Although dynamic information of the proposed tMRL technique in our study is somewhat limited by comparison, it can be performed without sedation or general anesthesia and is therefore less time consuming, less invasive and can be performed on an out-patient basis.
tMRL is an off-label use of the administered contrast agent.
Conclusion
Transpedal MR-lymphangiography is a new and valuable diagnostic tool in patients with chylous effusions scheduled for lymphatic interventions, providing information on the anatomy of central lymphatic. The leakage site, however, cannot be identified in all cases.Acknowledgements
No acknowledgement found.References
1. Shah RD, Luketich JD, Schuchert MJ et al. Postesophagectomy chylothorax: incidence, risk factors, and outcomes. Ann Thorac Surg 2012, 93(3):897-903
2. Cope C. Diagnosis and treatment of postoperative chyle leakage via percutaneous transabdominal catheterization of the cisterna chyli: a preliminary study. J Vasc Interv Radiol 1998, 9(5):727-34.
3. Cope C, Salem R, Kaiser LR. Management of chylothorax by percutaneous catheterization and embolization of the thoracic duct: prospective trial. J Vasc Interv Radiol 1999, 10(9):1248-54.
4. Schild H, Hirner A. Percutaneous translymphatic thoracic duct embolization for treatment of chylothorax. RoeFo 2001, 173(7):580-2.
5. Schild HH, Strassburg CP, Welz A et al. Treatment options in patients with chylothorax. Dtsch Arztebl Int 2013,110(48):819-26.
6. Schild HH, Naehle CP, Wilhelm KE, Kuhl CK, Thomas D, Meyer C, Textor J, Strunk H, Willinek WA, Pieper CC. Lymphatic Interventions for Treatment of Chylothorax. Rofo. 2015;187(7):584-8.
7. Kos S, Haueisen H, Lachmund U et al. Lymphangiography: forgotten tool or rising star in the diagnosis and therapy of postoperative lymphatic vessel leakage. Cardiovasc Intervent Radiol 2007, 30(5):968-73.
8. Matsumoto T, Yamagami T, Kato T et al. The effectiveness of lymphangiography as a treatment method for various chyle leakages. Br J Radiol 2009, 82(976):286-90.
9. Kawasaki R, Sugimoto K, Fujii M et al. Therapeutic effectiveness of diagnostic lymphangiography for refractory postoperative chylothorax and chylous ascites: correlation with radiologic findings and preceding medical treatment. Am J Roentgenol 2013, 201(3):659-66.
10. Krishnamurthy R, Hernandez A, Kavuk S, Annam A, Pimpalwar S. Imaging the central conducting lymphatics: initial experience with dynamic MR lymphangiography. Radiology. 2015;274(3):871-8.
Figures