3261
Insights from comprehensive fetal cardiovascular MRI assessment using 3D motion-correction and metric-optimised gated phase contrast in cases of suspected coarctation of the aorta1Division of Imaging Sciences and Biomedical Engineering, King's College London, London, United Kingdom, 2Department of Paediatric and Fetal Cardiology, Evelina London Children's Hospital, London, United Kingdom, 3Department of Computing (BioMedIA), Imperial College London
Synopsis
The antenatal diagnosis of coarctation of the aorta can be life saving; however, it is notoriously difficult to predict using ultrasound alone. We present 16 fetal cases with suspected coarctation of the aorta between 30-36 weeks, assessed using a combination of novel prenatal MRI techniques: three-dimensional motion corrected slice-volume registration and metric-optimised gated phase contrast flow measurements. Detailed 3D analysis revealed significant correlation between the size and position of the aortic isthmus and the need for neonatal surgical repair. Retrograde flow at the aortic isthmus and the angle of its insertion relative to the arterial duct may also be important variables. The comprehensive physiological data generated by combining novel fetal MRI techniques may offer powerful insights into traditionally challenging antenatal diagnoses.
Introduction
The antenatal diagnosis of severe neonatal coarctation of the aorta can be life-saving, affording the opportunity for affected babies to receive prompt treatment in specialist centres.1 However, the aetiology of the condition is poorly understood, and echocardiography - traditionally the only imaging modality available – is poorly sensitive.2 We sought to investigate how the combination of novel fetal cardiac MRI techniques might generate more comprehensive physiological profile in cases of suspected coarctation.
Methods
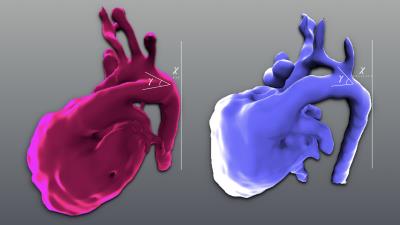
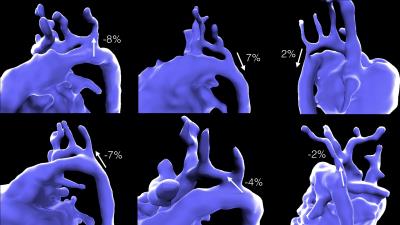
Referrals were encouraged directly from the clinical fetal cardiology service at the Evelina London Children’s Hospital, for any antenatal cases assessed by a fetal cardiologist in which coarctation was suspected. MRI evaluation consisted of up to twelve overlapping 2D single-shot fast spin echo sequences (Philips, 1.5T, TR = 20000, TE = 80ms, flip angle = 90 degrees, voxel size = 1.25 x 1.25mm, slice thickness = 2.5mm, SENSE, factor = 2, partial Fourier-factor 0.547, slice duration 546ms), processed using novel motion-corrected slice-volume registration techniques developed in our institution which generate highly detailed three-dimensional volumes of the fetal thorax.3,4,5 Multiple anatomical characteristics were then assessed, including both standard 2D echocardiographic parameters, and two novel parameters readily available from 3D data: the distance from the insertion of the aortic isthmus to the descending aorta, and the degree of angulation between the isthmus and the arterial duct (figure 1). In addition, fetal vascular flow rates were calculated in the ascending aorta, superior caval vein, pulmonary artery and descending aorta using metric-optimised gated phase contrast sequences, a technique that has been previously described.6Results
Sixteen fetuses were assessed, at a mean gestational age of 33 weeks (range 30–36 weeks). Anatomical measurements were acquired for all 16 patients, and flow measurements in 11 patients. Outcome data was collected up to four weeks after birth, classified as either surgical repair in the neonatal period (9 patients) or discharge without intervention (7 patients). Two parameters showed a significant correlation with early postnatal repair: the aortic isthmus:arterial duct ratio (0.47 vs 0.64; p = 0.04), and our novel measurement of the degree of proximal displacement of the aortic isthmus (1.13 vs 0.20; p <0.001). Trends were also observed towards the ductal-isthmal angle (53° vs 38°; p = 0.16), and flow rates (as percentage of combined ventricular output) in the ascending aorta (24% vs 29%; p = 0.09) and across the aortic isthmus (2.4% vs -2.2%; p = 0.17); however, these did not reach statistical significance in this preliminary study.Conclusion
We have demonstrated how the combination of novel fetal cardiovascular MRI techniques can provide a more comprehensive physiological assessment of the fetal circulation than is currently available using ultrasound alone. Applying this technology to traditionally challenging diagnoses such as coarctation of the aorta may provide important insights into pathophysiology of such conditions, and ultimately enhance our ability to provide an accurate prenatal diagnosis in affected patients.Acknowledgements
The authors acknowledge financial support the iFind Project (Wellcome Trust IEH Award 102431), and from the Department of Health via the National Institute for Health Research comprehensive Biomedical Research Centre award to Guy's and St Thomas' NHS Foundation Trust in partnership with King's College London and King's College Hospital NHS Foundation Trust.References
1. Franklin O, Burch M, Manning N, Sleeman K, Gould S, Archer N. Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbidity. Heart 2002; 87(1): 67-9.
2. Buyens A, Gyselaers W, Coumans A, et al. Difficult prenatal diagnosis: fetal coarctation. Facts, Views & Vision in ObGyn 2012; 4(4): 230-6.
3. Kainz B, Malamateniou C, Murgasova M, et al. Motion corrected 3D reconstruction of the fetal thorax from prenatal MRI. Med Image Comput Comput Assist Interv2014:284-291.
4. Kuklisova-Murgasova M, Quaghebeur G, Rutherford MA, Hajnal JV, Schnabel JA. Reconstruction of fetal brain MRI with intensity matching and complete outlier removal. Med Image Anal 2012; 16(8): 1550-64.
5. Lloyd D, Kainz B, van Amerom JFP et al; Proc. Intl. Soc. Mag. Reson. Med. 24 (2016); O413.
6. Jansz MS, Seed M, van Amerom JFP, et al. Metric optimized gating for fetal cardiac MRI. Magn Reson Med 2010; 64(5): 1304-14.
Figures