3234
Respiratory self-gated golden-angle spiral 4D flow MRI1Radiology, University Hospital of Cologne, Cologne, Germany, 2Healthcare, Philips GmbH, Hamburg, Germany
Synopsis
A spiral self-gated 4D Flow sequence is presented that operates at a predictable scan time. The respiratory self-navigation signal is extracted from the FID during the fat saturation pulse. The sequence allows to reconstruct 4D flow data in multiple respiratory states. This technique potentially allows to analyze respiratory dependent flow.
Introduction
4D flow has performed great advancement in becoming a clinically applicable tool1. Its long scan time and often limited SNR however, remain its major shortcomings. Especially breathing motion, which is typically addressed by gating approaches, can lead to unpredictable and long scan times. Spiral 4D flow has shown to be advantageous as compared to Cartesian 4D flow, due to its optimum k-space coverage, improved SNR and robustness against motion artefact. It is also known, that breathing motion has an effect on flow2, making a respiratory-resolved 4D flow acquisition of great interest. In this work, we present a self-gated golden-angle spiral 4D flow sequence which operates at a fixed and predictable scan time. 100% of the acquired data is exploited and re-binned into an arbitrarily defined number of cardiac and/or respiratory states. Different 4D flow datasets corresponding to different breathing motion states are generated.Methods
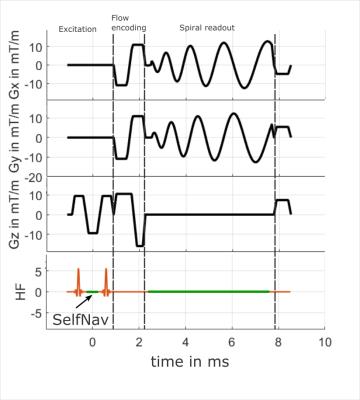
Acquisition: A stack of spiral acquisition with a golden-angle increment was used in combination with a 4-point non-symmetric flow encoding scheme3. The FID generated at every TR between the spatial-spectral excitation pulses was used as the self-gating signal (SelfNav)4. A sequence diagram is shown in figure 1. Data was acquired in a healthy volunteer on a 3T system (Philips, Best, the Netherlands) using a 32 channel cardiac array coil. The ECG and an abdominal air-cushion belt were recorded to monitor the heart and breathing motion, respectively. A field of view covering the aortic arch was acquired with following parameters: FOV: 280x280x50 mm³, resolution: 2.8x2.8x2.8 mm3, TE/TR = 2.4/9.2 ms, read-out time: 5 ms, venc = 150 cm/s. The scan time was fixed to 14:51 min resulting in a total number of 1053 different spokes per volume and flow encoding direction. Subsequent spokes were incremented by the golden angle of 222.4969° to ensure optimized volume coverage over time.
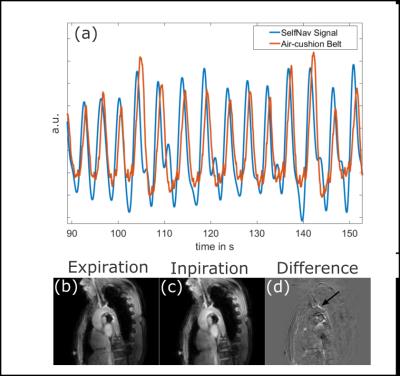
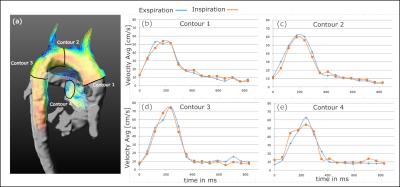
Reconstruction: The ECG signal was used to bin the data into cardiac phases and the SelfNav signal in the range of 0.1 to 0.5 Hz of the coil closest to the diaphragm was used as the breathing motion surrogate signal5,6. Data were then binned into 2 breathing states and 15 heart phases and resulting gaps were filled according to a nearest neighbor approach. Analysis: Net flow rates were extracted from 3 contours along the aortic arch and one contour in the main pulmonary artery, on both 4D flow reconstructions (inspiration and expiration).
Results
Figure 2 (a) shows the respiratory patterns extracted from the SelfNav signal compared to the air-cushion belt. Magnitude images of two respiratory states and their difference are shown in figure 2 (b,c,d). Figure 3 (a) illustrates the contour positions while figure 3 (b-e) shows the resulting flow curves for each of the planes in the two breathing states.Discussion
We have presented a spiral self-gated 4D flow acquisition technique in combination with a re-binning approach. The respiratory signal from the SelfNav signal is in line with the recorded belt signal. We demonstrated that a prospective breathing motion compensation (gating) can be avoided leading to a more predictable scan time. Respiratory-resolved 4D flow acquisitions were successfully reconstructed and analyzed.Conclusion
The freedom of re-binning the data into different breathing states offers the possibility to analyze respiratory-dependent flow. Due to the high temporal frequency of the SelfNav signal, the extraction of the ECG is planned in future work. A combination with an undersampling technique is warranted and would allow shorter scan times or improved temporal resolutions.Acknowledgements
No acknowledgement found.References
1. Dyverfeldt, P., et al., 4D flow cardiovascular magnetic resonance consensus statement. J Cardiovasc Magn Reson, 2015. 17(1): p. 72.
2. Johansson, B., S.V. Babu-Narayan, and P.J. Kilner, The effects of breath-holding on pulmonary regurgitation measured by cardiovascular magnetic resonance velocity mapping. J Cardiovasc Magn Reson, 2009. 11: p. 1.
3. Pelc, N.J., et al., Encoding strategies for three-direction phase-contrast MR imaging of flow. J Magn Reson Imaging, 1991. 1(4): p. 405-13.
4. Ingle, R.R., et al., Self-gated fat-suppressed cardiac cine MRI. Magn Reson Med, 2015. 73(5): p. 1764-74.
5. Buehrer, M., et al., Prospective self-gating for simultaneous compensation of cardiac and respiratory motion. Magn Reson Med, 2008. 60(3): p. 683-90.
6. Uribe, S., et al., Four-dimensional (4D) flow of the whole heart and great vessels using real-time respiratory self-gating. Magn Reson Med, 2009. 62(4): p. 984-92.
Figures