3233
Respiratory Controlled Adaptive K-space Reordering (ReCAR) Improves 4D Flow Image Quality1Siemens Healthcare, Columbus, OH, United States, 2Application Development, Siemens Healthcare, Erlangen, Germany, 3Siemens Healthcare, Chicago, IL, United States, 4Department of Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 5Department of Biomedical Engineering, Northwestern University, Chicago, IL
Synopsis
4D flow normally uses respiratory gating to mitigate breathing artifacts for thoracic and abdominal applications. Respiratory Controlled Adaptive k-space Reordering (ReCAR) employs k-space reordering based on the current respiratory position. It has been reported to increase respiratory gating efficiency for 4D flow applications. The purpose of this study was to systematically compare the image quality of 4D flow data acquired with and without adaptive k-space reordering.
Purpose
4D flow MRI provides comprehensive evaluation of cardiovascular hemodynamics by acquiring three-dimensional (3D) data combined with time-resolved velocity encodings in all three spatial directions (1). Due to its long acquisition time, respiratory gating is normally used to mitigate breathing artifacts (blurring, ghosting) for thoracic and abdominal applications. Respiratory Controlled Adaptive k-space Reordering (ReCAR), employing phase encoding k-space reordering based on the current respiratory position, has been reported to increase respiratory gating efficiency for 4D flow applications (2,3). The purpose of this study was to systematically compare the image quality of 4D flow data acquired with and without ReCAR.
Methods
Nine normal volunteers were enrolled in the study. Six volunteers were scanned on a 1.5T system (Siemens MAGNETOM Aera) and three on a 3 T system (Siemens MAGNETOM Skyra) with a body matrix and a spine coil for signal reception. 4D flow data was acquired using a navigator (NAV) gated 3D phase contrast gradient echo sequence with interleaved three-directional velocity encodings during free-breathing. ReCAR k-space ordering was based on the NAV detected respiratory position. Central k-space was acquired at end-expiration when respiratory displacement was minimal and outer k-space was acquired during inspiration (Figure 1b). Because end-expiration lasts slightly longer than end-inspiration and has less variability, a large portion of central k-space can be acquired at a consistent respiratory position, thereby reducing ghosting and respiratory artifacts. Non-ReCAR acquisitions were performed using linear k-space ordering. Typical imaging parameters were: TE/TR = 2.4/5.2 ms, temporal resolution = 41.6 ms, spatial resolution = 3.0×2.3×2.5 mm3, BW = 445 Hz/Pixel, FA = 7°, PAT = 2 with 24 integrated reference lines, VENC = 150 cm/s for all three velocity encodings, width of NAV acceptance window = 8 mm. The total acquisition time depends on heart rate, and navigator efficiency and was on the order of 10 to 12 min. In each volunteer, 4D flow images were acquired to cover the entire thoracic aorta and the proximal parts of the supra-aortic branches. The scans were repeated twice without and with ReCAR. Image quality was scored independently by two experienced observers blinded to image acquisition strategy using a 4-point scoring system based on artifact level (Table 1).
Results
Figure 1 shows the respiratory position map of (ky, kz) from one 4D flow dataset acquired without and with ReCAR, in which red represents data acquired during expiration and blue represents data acquired during inspiration. In ReCAR, a large portion of central k-space was acquired at a consistent expiration position, while the outer part of k-space is acquired during inspiration with more variation. Although there were physiological variations during image acquisition, the mean acceptance rate for 4D flow acquired without and with ReCAR were not significantly different (72 ± 16% vs. 78.1 ± 16.8%, p = 0.176). Figure 2 and Figure 3 show representative examples of magnitude and phase images from the center of the aorta in the peak systole acquired without and with ReCAR at 1.5T and 3T. Compared to ReCAR, the signal was less homogeneous within the aorta and more ghosting artifacts were observed (arrows) in the images acquired using NAV gating only. The image quality scores from both reviewers are summarized in Table 2. The image quality was significantly better for gate + ReCAR.
Conclusion
Compared to images acquired with NAV gating only, ReCAR significantly improved the 4D flow image quality and reduced artifacts by adapting the k-space acquisition order based on the respiratory position sampled by navigator pulses without increasing the total scan time. Due to its increased robustness against respiratory motion, ReCAR may enable wider acceptance windows and effectively speed up 4D flow acquisitions.
Acknowledgements
No acknowledgement found.References
(1) Markl M, Frydrychowicz A, Kozerke S, Hope M, Wieben O. 4D flow MRI. J Magn Reson Imaging.2012;36:1015–1036.
(2) Markl M, Harloff A, Bley TA, et al. Time-resolved 3D MR velocity mapping at 3T: Improved navigator-gated assessment of vascular anatomy and blood flow. J Magn Reson Imaging 2007;25:824 –831.
(3) Bailes DR, Gilderdale DJ, Bydder GM, et al. Respiratory ordered phase encoding (ROPE): method for reducing respiratory motion artifacts in MR imaging. J Comput Assist Tomogr 1985; 9: 835-838.
Figures
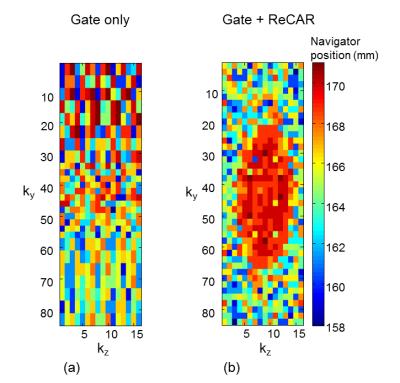
Figure 1. Respiratory position map of (ky, kz) from one 4D flow dataset acquired without (a) and with ReCAR (b), in which red represents data acquired during expiration and blue represents data is acquired during inspiration.
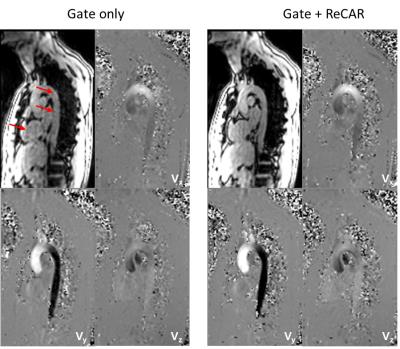
Figure 2. Example of magnitude and phase images from the center of the aorta in peak systole acquired without and with ReCAR at 1.5T. Arrows show the artifacts.
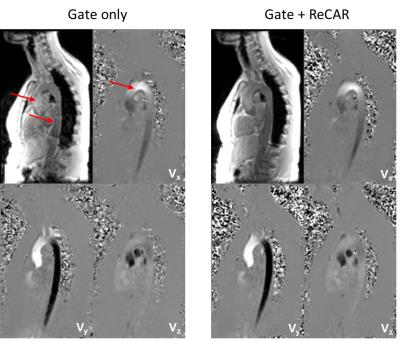
Figure 3. Example of magnitude and phase images from the center of the aorta in systole acquired without and with ReCAR at 3T. Arrows show the artifacts.
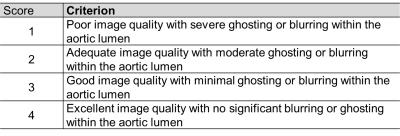
Table 1. Scoring Criteria.
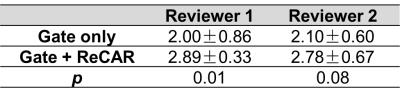
Table 2. Image Quality Score