3211
Diagnosis of Liver Cirrhosis Using Morphological Score with Magnetic Resonance Laparoscopy1Department of Radiology, University of Yamanashi, Japan, Yamanashi, Japan
Synopsis
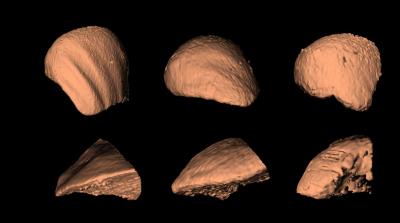
Liver biopsy is a gold standard for the diagnosis of liver cirrhosis. However, biopsy can be false negative because of small amount of tissue sampled. Laparoscopy has been also used as another gold standard for the diagnosis of cirrhosis by directly assessing the liver surface, which compensate for the limitation of biopsy. Laparoscopy like 3D image can be obtained by 3D reconstruction of gadoxetic acid-enhanced hepatobiliary phase images (MR laparoscopy). The two MR laparoscopy findings, i.e. the rib pitting of liver surface and the sharpness of edge, showed good performance for discriminating liver cirrhosis from non-cirrhosis.
Purpose
Laparoscopic evaluation of the liver surface has been one of the gold standard for the diagnosis of liver cirrhosis, because cirrhotic liver has specific surface appearance. Similarly, morphological assessments on cross sectional images including ultrasonography and computed tomography (CT) is supposed to be useful for suggesting liver cirrhosis.1-3 The details of liver surface can be assessed with 3D reconstruction of the liver MRI, MR laparoscopy. The purpose of this study was to evaluate the utility of MR laparoscopy discriminating liver cirrhosis from non-cirrhosis.Methods
<Patients and data acquisition> This retrospective study included 65 patients who underwent gadoxetic acid-enhanced liver images using 3.0T MR system (Discovery MR750, GE Healthcare, Japan) between March and September 2016 and were confirmed the histopathological stage of hepatic fibrosis (METAVIR scoring system4) by fine needle biopsy (n = 8) or surgical resection (n = 57). For MR laparoscopy, the protocol of image acquisition was as following; 3D FSPGR sequence with fat suppression; flip angle, 25˚; TR/TE, 4.7 and 1.8; slice thickness, 2mm; respiratory gating with navigator echo on the right side of diaphragm; image matrix, 512 x 512; the field of view, 33.4 x 32.0 cm. MR laparoscopy was performed with three-dimensional shaded surface rendering of hepatobiliary phase images using a work-in-progress workstation (Synapse Vincent, Fujifilm Medical, Japan) (Figure 1). Rib pitting of liver surface (grade 1, clear; 2, faint; and 3, none) and sharpness of edge (grade 1, sharp; 2, slightly round; and 3, round) were evaluated with three-point grades based on the findings of MR laparoscopy (Figure 2). Morphological score (scores 2 ‒ 6) was defined by adding the two grades. MRE was obtained with a vibrator placed outside of the MR room. A 2D gradient-echo sequence in the transverse plane was used to obtain images for MRE. The scanning position was set above the gallbladder and below the subphrenic region of the liver. A section thickness of 10 mm was applied. Other MR parameters were; TR/TE, 50 and 20; flip angle, 23°; number of signals acquired, 1; the field of view, 30–34 x 40–45 cm; the matrix size, 256 x 80; the acquisition time, 17 s (3.0T); and the axis of the motion-sensitizing gradient pulse, the z-axis. The frequency of the driver was 60 Hz, and the amplitude was 60%. As a rule of region of interest (ROI) placement, the ROI was at least 1.5 cm2 and excluded the blood vessels, the liver edge, and areas where inference with the propagating waves was observed on the phase images.
<Analysis> The diagnostic performance of morphological score for discriminating liver cirrhosis from non-cirrhosis was assessed by Wilcoxon rank sum test and receiver operating characteristic (ROC) analysis. Morphological score was compared with the liver stiffness measured with MR elastography (MRE). Serum alanine aminotransferase (ALT) level, which represent inflammatory activity in the liver, was retrieved from medical record system. The software for statistical analyses was R (version 3.2.3).
Results
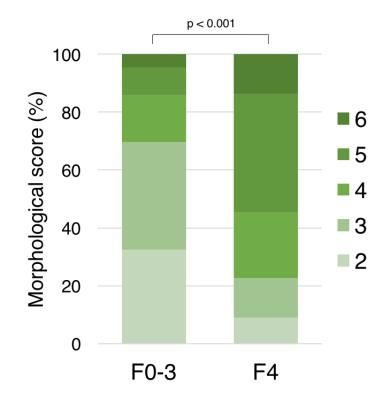
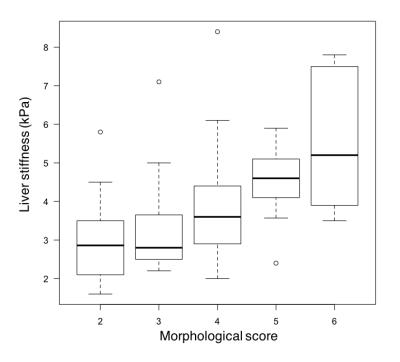
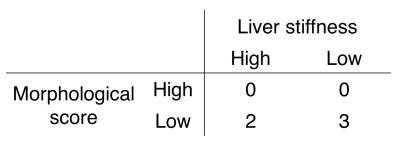
The morphological score in F4 (mean 4.36, n = 22) was significantly higher than that in F0-3 (mean 3.16, n = 43) (p <0.001) (Figure 3). The area under the ROC curve was 0.77 (95% confidence interval, 0.64-0.89). Using score 4.5 as the cut-off value, the sensitivity and specificity for discriminating F4 were 55% (12/22) and 86% (37/43). Morphological score showed good correlation with liver stiffness (r = 0.51) (Figure 4). We found 5 cases with fibrosis stage of F0-3 and high serum ALT level (high inflammatory activity in the liver). Two of the 5 cases were over-estimated by MRE (5.0 kPa and 5.8 kPa, >4.4 kPa was the cutoff value to indicate cirrhosis in our series), while all cases were correctly categorized as non-cirrhosis by MR laparoscopy (morphological score = 2 - 4) (Figure 5).Discussion
This study showed that MR laparoscopy was able to discriminate cirrhosis from non-cirrhosis with good accuracy. As shown in the previous publications, MRE showed solid utility for the evaluation of cirrhosis. However, MRE has a limitation in the liver with inflammation, i.e. inflammation is a major confounder of cirrhosis in MR elastography5. Although the diagnostic performance of MR laparoscopy is not as great as that of MRE, MR laparoscopy may have an advantage in the cases with active inflammation in the liver. MRE and MR laparoscopy may compensate their limitations one another.Conclusion
The evaluation of the morphological score with MR laparoscopy showed good diagnostic performance for liver cirrhosis.Acknowledgements
No acknowledgement found.References
1. Cao G, Shi P, Hu B. Liver fibrosis identification based on ultrasound images captured under varied imaging protocols. J Zhejiang Univ Sci B. 2005;6(11):1107-1114.
2. Smith AD, Branch CR, Zand K, et al. Liver Surface Nodularity Quantification from Routine CT Images as a Biomarker for Detection and Evaluation of Cirrhosis. Radiology. 2016;280(3):151542.
3. Chen Y-W, Luo J, Dong C, et al. Computer-aided diagnosis and quantification of cirrhotic livers based on morphological analysis and machine learning. Comput Math Methods Med. 2013;2013:264809.
4. Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996;24(2):289-293.
5. Ichikawa S, Motosugi U, Nakazawa T, et al. Hepatitis activity should be considered a confounder of liver stiffness measured with MR elastography. J Magn Reson Imaging. 2015;41(5):1203-1208.
Figures