3194
Gadoxetic acid-enhanced MRI findings as a risk of multicentric recurrence of hepatocellular carcinoma after hepatectomy1Radiology, University of Yamanashi, Chuoh-shi, Japan, 2First surgery, University of Yamanashi, Chuoh-shi, Japan
Synopsis
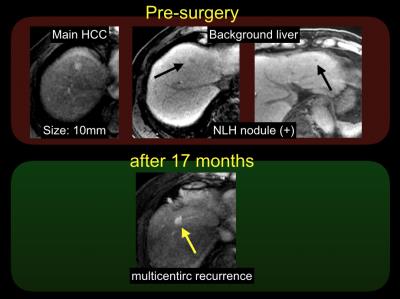
Nodules of non-hypervascular and low signal intensity during hepatobiliary phase (NLH nodules) detected by gadoxetic acid-enhanced magnetic resonance imaging (EOB-MRI), also known as hypovascular hypointense nodules, is important MR features that indicate the hepatocellular carcinoma (HCC) development in the future. The presence of NLH nodules is known as at high risk of HCC development in the liver. Hence, we hypothesized that NLH nodules can be also a risk of recurrence after surgical resection of HCCs. We evaluated the prognostic value of NLH nodules in patients with HCC. Presence of NLH nodules is at high risk of multicentric recurrence after hepatectomy.
Purpose
It is known that there are 2 types of recurrence after the treatment of HCC; i) intra-hepatic metastases recurrence (that typically occurs within a year after surgery) and ii) multicentric recurrence. Intra-hepatic metastases recurrence means a metastasis from the HCC, which was treated with locoregional therapy. The risk of intra-hepatic metastases recurrence depends on the tumor characteristics such as tumor grade, the size of the tumor, or ADC value1). Multicentric recurrence is a metachronous carcinogenesis in the remnant liver. A risk of multicentric recurrence means the risk of hepatocarcinogenesis from the liver. It is important to distinguish these two types of recurrence, because intra-hepatic metastases recurrence suggests that the treatment of HCC did not succeed and the tumor cells can be already spread out in the blood. On the other hand, the multicentric recurrence indicate that the newly developed HCC is not related to the former HCC, which means we can treat the new HCC as we treated the first HCC. It is well known that liver stiffness and presence of NLH nodule are at high risk of hepatocarcinogenesis. Therefore, we hypothesized that these MR features can be a risk of multicentric recurrence in patients with HCC treated with surgery. The purpose of this study was to evaluate the prognostic values of MR features including liver stiffness by MR elastography (MRE) and the presence of NLH nodules detected by EOB-MRI for predicting multicentric recurrence after surgery in HCC.Methods
By searching a medical record in our institution, we found 124 consecutive patients with hypervascular HCC who had undergone heaptectomy as well as pre-operative EOB-MRI within 5 months. After excluding patients with early recurrence (<1 year), we finally included 95 patients. Preoperative patient characteristics (age, sex, and any underlying liver disease) and imaging features (tumor size, number, liver stiffness measured by MRE, and the presence of NLH nodules) were evaluated to predict multicentric recurrence using Cox proportional hazards regression analysis, which was used to assess disease-free survival. In this study, multicentric recurrence was defined as a recurrent event that occurs more than 1 year after surgery. Kaplan-Meier analysis was used to compare the prognosis between the groups with and without early recurrence.Results
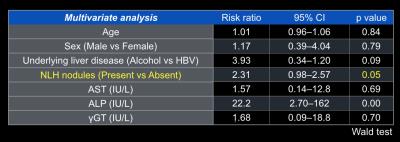
The median follow-up period was 36.9 months. During the follow up period, 28 patients (22.6%) developed multicentric recurrence after surgery. The univariate analyses revealed that the presence of NLH nodules was significantly associated with disease-free survival (P = 0.03). Multivariate logistic regression analysis with NLH nodules, age, and sex showed that the presence of NLH nodules (P = 0.05) was an independent predictor of disease-free survival. The results of Kaplan-Meier analysis revealed that patients with NLH nodules had a significantly worse prognosis than those without NLH nodules (P = 0.04). Five years after the surgery, the disease-free survival of patients with NLH nodules and without NLH nodules was 28.3% and 65.2%, respectively.Discussion
The previous study suggested that NLH nodules, or non-hypervascular hypointense nodules, was an independent risk factor of recurrence after hepatectomy2). Our results were consistent with their results. The risk ratio shown in their paper was almost same as ours. Also, Liver fibrosis is supposed to be a strong indicator of HCC development. In our study, the p value of MRE was 0.08, which was close to the significant level. It was probably because of the small number of patients we included in our study.Conclusion
The presence of NLH nodules detected by EOB-MRI is an indicator of HCC recurrence and worse prognosis after surgical resection of HCCs.Acknowledgements
No acknowledgement found.References
1) Toyoda H, et al. J Hepatol 2013; 63: 145-50
2) Muhi A, et al. Hepatol Int 2013;7:662-668.
Figures