3189
Radiologic-Pathologic Correlation and MR Analysis of Hepatocellular Adenoma Subtypes.1Radiology, Mayo Clinic Arizona, Scottsdale, AZ, United States, 2University of Pennsylvania, PA, United States, 3Pathology, Mayo Clinic Arizona, Scottsdale, AZ, United States
Synopsis
Hepatocellular adenomas (HCA) present as four genetic
subtypes that vary greatly in their clinical behavior and MR appearance. Inflammatory HCA has the highest
propensity for hemorrhage, is characterized by hyperintense T2 signal, and
displays arterial hyper-enhancement that persists on portal venous and delayed
phases. HNF1-alpha mutated HCA
portends a good prognosis, and is characterized by diffuse intracellular
lipid. Beta-catenin HCA is less common and difficult to diagnose on
imaging, though arguably the most important because of its high likelihood for
malignant transformation. Unclassified HCA is not well understood in
terms of imaging or clinical significance.
Purpose and Background Information
Purpose
Hepatocellular adenomas are often considered "benign" tumors; however, their propensity to hemorrhage and undergo malignant degeneration significantly impacts patient management. Historically these tumors were diagnosed with percutaneous biopsy or surgery because of the widely variable imaging appearance. Furthermore, even with a pathologically proven diagnosis it was difficult to predict which tumors were "bad actors". Over the last decade, technical advances have permitted identification of specific histopathologic and genetic features that help predict tumor behavior. Based upon these findings, four subgroups of hepatocellular adenoma were characterized, each with a unique MRI appearance. Through a retrospective analysis of 65 patients with pathologically proven hepatocellular adenoma from 1/1/2010-present, we will demonstrate several MRI examples from each category and discuss the clinical implications of each subgroup.
Outline and content
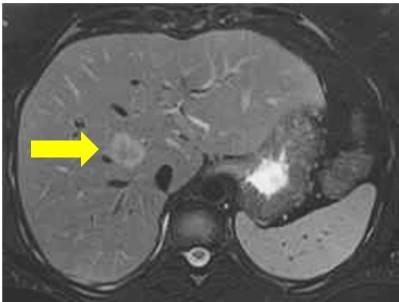
Inflammatory HCA:
Clinical features
Most common subtype
OCPs and obesity are risk factors
Can present with syndrome including fever, leukocytosis, as well as elevated liver function tests and inflammatory markers
Highest propensity for hemorrhage and small risk of malignant transformation (approx. 10%)
Imaging features
Noncontrast: Diffusely T2 hyperintense T1 iso to slightly hyperintense
Intense arterial enhancement with persistent portal venous and delayed enhancement
No diffuse signal drop on opposed phase (may have focal signal drop)
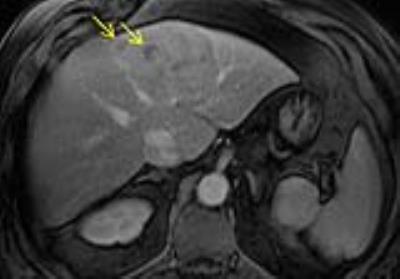
HNF1-alpha mutated HCA:
Clinical features
Second most common subtype
Occurs exclusively in females, 90% with history of OCP use
Most favorable prognosis (lowest risk for hemorrhage and malignancy of all adenomas)
Imaging features
Noncontrast: T2 isointense to slightly hyperintense T1 isointense or hyperintense
Moderate arterial enhancement without persistent portal venous and delayed enhancement
Diffuse signal drop on opposed phase
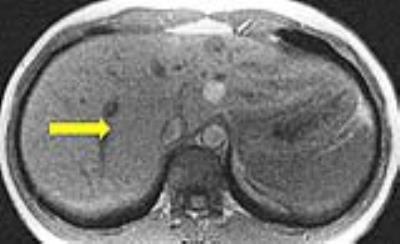
Beta-catenin HCA:
Clinical features
Third most common subtype
Highest association with malignant transformation
Occur more frequently in men and are associated with exogenous male hormone administration
Association with glycogen storage disease and Familial Adenomatosis Polyposis syndrome
Imaging features:
No consistent imaging features
May show vague central scar
May mimic hepatocellular carcinoma (strong arterial enhancement with washout)
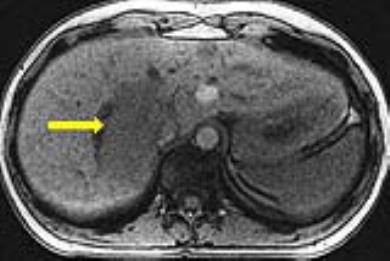
Unclassified HCA - No consistent clinical or imaging features (least common subtype)
Summary
By improving our ability to detect and sub-classify hepatocellular adenomas at MRI, we hope to better inform our hepatology and surgical colleagues and significantly impact patient management.
Acknowledgements
No acknowledgement found.References
Edmondson HA, Henderson B, Benton B. Liver-cell adenomas associated with use of oral contraceptives. N Engl J Med 1976; 294: 470–472.
Zucman-Rossi J, Jeannot E, Nhieu JT et al. Hepatology. 2006 Mar;43(3):515-24. Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC.
Luigi Grazioli, Maria Pia Bondioni, Hiroki Haradome et al. Hepatocellular Adenoma and Focal Nodular Hyperplasia: Value of Gadoxetic Acid–enhanced MR Imaging in Differential Diagnosis. Radiology 2012 262:2, 520-529.
Cherqui D, Rahmouni A, Charlotte F, et al. Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology 1995;22(6):1674–1681. CrossRef, Medline
Andrei S. Purysko, Erick M. Remer, Christopher P. Coppa. Characteristics and Distinguishing Features of Hepatocellular Adenoma and Focal Nodular Hyperplasia on Gadoxetate Disodium–Enhanced MRI. AJR 2012; 198:115–123.
Sheela Agarwal, Jorge M. Fuentes-Orrego, Thomas Arnason et al. Inflammatory Hepatocellular Adenomas Can Mimic Focal Nodular Hyperplasia on Gadoxetic Acid–Enhanced MRI. AJR October 2014, Volume 203, Number 4.
Miller FH, Hammond N, Siddiqi AJ, et al. Utility of diffusion-weighted MRI on distinguishing benign and malignant hepatic lesions. J Magn Reson Imaging 2010; 32:138–14.
Matthew D. F. McInnes, MD, FRCPC, Rebecca M. Hibbert, MD, FRCPC, João R. Inácio, MD Nicola Schieda, MD, FRCPC. Focal Nodular Hyperplasia and Hepatocellular Adenoma: Accuracy of Gadoxetic Acid–enhanced MR Imaging—A Systematic Review. Radiology: Volume 277: Number 2—November 2015.
Grieser C, Steffen IG, Kramme IB, et al. Gadoxetic acid enhanced MRI for differentiation of FNH and HCA: a single centre experience. Eur Radiol 2014;24(6):1339–1348.
Luigi Grazioli, MD, Maria Pia Bondioni, MD, Hiroki Haradome, MD et al. Hepatocellular Adenoma and Focal Nodular Hyperplasia: Value of Gadoxetic Acid–enhanced MR Imaging in Differential Diagnosis. Radiology: Volume 262: Number 2—February 2012.
Tse JR, Naini BV, Lu DS, Raman SS. Qualitative and Quantitative Gadoxetic Acid-enhanced MR Imaging Helps Subtype Hepatocellular Adenomas. Radiology 2016 Apr;279(1):118-27. Epub 2015 Oct 27.
Katabathina VS, Menias CO, Shanbhogue, AKP, Jagirdar J, Paspulati RM, Prasad SR. Genetics and imaging of hepatocellular adenomas: 2011 update. RadioGraphics 2011; 31(6):1529–1543.
Khanna M, Ramanathan S, Fasih N, Schieda N, Virmani V, McInnes MD. Current updates on the molecular genetics and magnetic resonance imaging of focal nodular hyperplasia and hepatocellular adenoma. Insights Imaging 2015 Jun;6(3):347-62. Epub 2015 Mar 20.14.
Belghiti J, Cauchy F, Paradis V, Vilgrain V. Diagnosis and management of solid benign liver lesions. Nat Rev Gastroenterol Hepatol 2014 Dec;11(12):737-49. 15.
De Kock I, Mortelé KJ, Smet B, Gillardin P, Pauwels W, De Backer AI. Hepatic adenomatosis: MR imaging features. JBR-BTR. 2014 Mar-Apr;97(2):105-8.
Agrawal S, Agarwal S, Arnason T, Saini S, Belghiti J. Management of Hepatocellular Adenoma: Recent Advances. Clin Gastroenterol Hepatol. 2015 Jul;13(7):1221-30. Epub 2014 Jun 5.
Thomeer MG, E Bröker ME, de Lussanet Q, Biermann K, Dwarkasing RS, de Man R, Ijzermans JN, de Vries M. Genotype-phenotype correlations in hepatocellular adenoma: an update of MRI findings. Diagn Interv Radiol. 2014 May-Jun;20(3):193-9.
Thomeer MG, Willemssen FE, Biermann KK, et al. MRI features of inflammatory hepatocellular adenomas on hepatocyte phase imaging with liver-specific contrast agents. J Magn Reson Imaging. 2014 May;39(5):1259-64. Epub 2013 Jul 29.
Figures