3167
The IASLC/ ITMIG Thymic Epithelial Tumor Staging: Comparison of Staging Capability among Whole-Body PET/MRI, MRI including DWI, PET/CT and Conventional Radiological Examination1Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Advanced Biomedical Imaging Research Center, Kobe University Graduate School of Medicine, Kobe, Japan, 3Division of Radiology, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 4Center for Medical Research and Development, Toshiba Medical Systems Corporation, Otawara, Japan, 5MR Clinical Solution department, Toshiba Medical Systems Corporation, Otawara, Japan, 6Center for Radiology and Radiation Oncology, Kobe University Hospital, Kobe, Japan
Synopsis
Accurate stage assessment is essential for choosing the appropriate treatment strategy for thymic epithelial tumor patients. Recently, the International Association for the Study of Lung Cancer (IASLC) and International Thymic Malignancies Interest Group (ITMIG) proposed a new IASLC/ITMIG thymic epithelial tumor stage classification system. The purpose of this study was to compare the diagnostic capability for the IASLC/ ITMIG thymic epithelial tumor staging among whole-body FDG-PET/MRI, MRI, FDG-PET/CT and conventional radiological examinations based on guidelines.
Introduction
Accurate stage assessment is essential for choosing the appropriate treatment strategy for thymic epithelial tumor patients. Conventional radiological examination including whole-body contrast-enhanced (CE-) CT as well as conventional MRI has been applied in routine clinical practice. In the last decade, diffusion-weighted imaging (DWI) has been tested for demonstration of the utility for management of thymic epithelial tumor as well as lung cancer (1-4). Moreover, whole-body FDG-PET/CT, MRI including DWI and PET/MRI have also been suggested as useful in various oncologic patients. Recently, the International Association for the Study of Lung Cancer (IASLC) and International Thymic Malignancies Interest Group (ITMIG) proposed a new IASLC/ITMIG thymic epithelial tumor stage classification system (5). However, no direct comparisons for diagnostic capability for the IASLC/ ITMIG thymic epithelial tumor staging among whole-body PET/CT, whole-body PET/ MRI, whole-body MRI and conventional radiological examination in thymic epithelial tumor patients.
We hypothesized that whole-body FDG-PET/MRI and MRI have better potential for diagnosis of the IASLC/ ITMIG thymic epithelial tumor staging than conventional radiological examination including whole-body CE-CT, CE-brain MRI and bone scintigraphy, and are considered at least as valuable as whole-body FDG-PET/CT.
The purpose of this study was to compare the diagnostic capability for the IASLC/ ITMIG thymic epithelial tumor staging among whole-body FDG-PET/MRI, MRI, FDG-PET/CT and conventional radiological examinations based on guidelines.
Materials and Methods
64 consecutive and pathologically diagnosed thymic epithelial tumor patients (30 men, 34 women; mean age 56 years) prospectively underwent whole-body MRI, integrated PET/CTs, conventional radiological examination, surgical resection, pathological examination, and more than 2-year follow-up examinations. All whole-body MRI including DWI were obtained by using a 3T MR system (Vantage Titan 3T, Toshiba Medical Systems) with multi-channel whole-body coil as having parallel imaging capability (Atlas SPEEDER coil, Toshiba). All co-registered MR/PETs were generated by means of our proprietary software. The final IASLC/ ITMIG thymic epithelial tumor staging in each patient was determined based on tumor board reviewing all examination results. Then, T, N and M factors as well as tumor stage in each patient were prospectively assessed by all methods.
To evaluate interobserver agreement of each factor on all methods, weighted kappa statistic was used. To evaluate agreements of all factors and stage between each method based on consensus reading and final diagnosis, kappa statistics were also performed. Diagnostic accuracy of each factor and clinical stage were also statistically compared each other by using McNemar’s test. Agreements were considered as poor for κ< 0.21, fair for κ = 0.21–0.40, moderate for κ = 0.41–0.60, substantial for κ = 0.61–0.80, and excellent for κ = 0.81–1.00. A p value < 0.05 was considered statistically significant for all statistical analyses.
Results
Representative case is shown in Figure 1 and 2.
Interobserver agreement on each method was assessed as almost perfect on T and M factors (0.69<κ<1.00), and substantial or almost perfect on N factor (0.67<κ< 0.86).
Agreement of staging between final diagnosis and each method and staging accuracy of each method are shown in Figure 3. Although agreements of PET/CT (κ=0.56) and conventional radiological examination (κ=0.43) were moderate, that of whole-body PET/CT (κ=0.71) and MRI (κ=0.71) were determined as substantial. In addition, staging accuracy of PET/MRI (84.4%) and MRI (84.4%) were significantly higher than that of conventional radiological examination (71.9%, p<0.05).
Conclusion
Whole-body PET/MRI and MRI have better potential for the IASLC/ ITMIG thymic epithelial tumor staging than conventional radiological examination, and are considered at least as valuable as PET/CT with CE-brain MRI in this setting.Acknowledgements
This work was financially and technically supported by Toshiba Medical Systems, and financially supported by Bayer Pharma.References
1. Ohno Y, Koyama H, Onishi Y, et al. Radiology. 2008; 248(2): 643-654.
2. Takenaka D, Ohno Y, Matsumoto K, et al. J Magn Reson Imaging. 2009; 30: 298-308.
3. Seki S, Koyama H, Ohno Y, et al. Eur J Radiol. 2014; 83: 835-842.
4. Ohno Y, Koyama H, Yoshikawa T, et al. Radiology. 2015; 275: 849-861.
5. Detterbeck FC, Stratton K, Giroux D, et al; Staging and Prognostic Factors Committee; Members of the Advisory Boards; Participating Institutions of the Thymic Domain. J Thorac Oncol. 2014; 9(9 Suppl 2): S65-72.
Figures
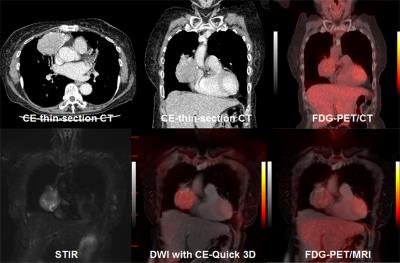
Figure 1. 72-year-old female patient with thymoma type AB (pT2N0M0: pStage II)
Anterior mediastinal tumor diagnosed as thymoma type AB is demonstrated on all methods, and pericardial invasion is suspected on all methods. This patient was assessed as clinical stage as stage II (T2N0M0), and accurately diagnosed, when compared with pathological stage.
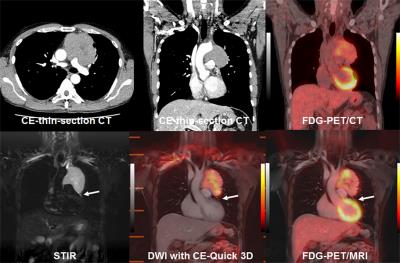
Figure 2. 54-year-old male patient with thymoma type B1 (pT4N0M1a: pStage IVa)
Anterior mediastinal tumor diagnosed as thymoma type B1 is suspected the main pulmonary artery on all methods. In addition, STIR, DWI with CE-Quick 3D and PET/MRI also suspect separate pericardial nodule (arrow). This patient was assessed as clinical stage as stage IIIb (T4N0M0) on PET/CT and conventional radiological examination, and as stage IVa (T4N0M1a) on whole-body PET/MRI and MRI. According to pathological examination, this patient was accurately diagnosed on whole-body PET/MRI and MRI.
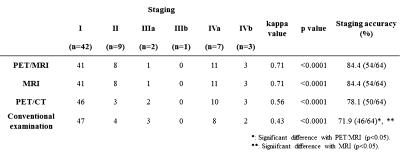
Figure 3. Agreement between final diagnosis and stage evaluation by each method and staging capability on each method.
Agreements of PET/CT (κ=0.56) and conventional radiological examination (κ=0.43) were moderate, although that of whole-body PET/CT (κ=0.71) and MRI (κ=0.71) were determined as substantial. In addition, staging accuracy of PET/MRI (84.4%) and MRI (84.4%) were significantly higher than that of conventional radiological examination (71.9%, p<0.05).