3160
The impact of heterogeneity on regurgitation classification for pulmonary artery after repaired Tetralogy of Fallot1Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, United States, 2Institute of Biomedical Electronics and Bioinformatics, National Taiwan University, Taipei, Taiwan, 3Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, 4Computer Science and Engineering, National Sun Yat-Sen University, Kaohsiung, Taiwan
Synopsis
The degree of pulmonary regurgitation has been a determinant for re-intervention for patients with repaired TOF. However, in practice, the accurate assessment of regurgitation may be interfered by the simultaneous existence of forward flow and backward flow in any single cardiac phase, which may mislead clinical decision making. In this study, we investigated the impact of heterogeneity in blood flow profiles on guiding management and the classification of regurgitation. Preliminary results suggest that pixel-wise reexamination may be required for reclassification, especially for patients with marginal moderate regurgitant fraction value.
Introduction
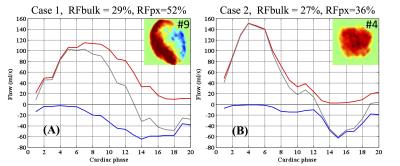
Quantitative flow analysis derived from PC-MRI has been recognized as a reliable noninvasive modality for long-term follow-up after surgical repair of Tetralogy of Fallot (TOF).1 To distinguish the degree of pulmonary regurgitation, regurgitant fraction (RF) has been introduced as a significant determinant for re-intervention. Recently, studies have reported that a number of technical and clinical sources of error encountered in PC-MRI flow measurements may lead to false clinical decision.2 For flow pattern in TOF, it is considered that forward flow appears during systolic periods while backward flow occurs during diastole, however in practice, regurgitant flow may initiate during the systole periods (Fig. 1). The effect of partial backward flow during systole period may impair the accuracy assessment of residual pulmonary regurgitation, and therefore, interfere with the guiding management. In this study, the purpose was aimed at evaluating the impact on clinical decision making and the classification of regurgitation when backward flow occurred during systolic periods. The preliminary results demonstrated that the amount of regurgitation levels was underrated with conventional estimates, suggesting that the pixel-wise reexamination may be required for reclassification.Methods
Imaging was performed on a 1.5T General Electric Signa CV/i system. PC-MR images of main/left/right pulmonary artery (MPA/LPA/RPA) were obtained with retrospective ECG gating for patients after repaired TOF. Flow velocity of 20 time phases per cardiac cycle was measured with VENC set as 200 cm/sec. Quantitative flow parameters, including forward flow volume (FFV) and backward flow volume (BFV), were then estimated by two approaches: the conventional time-averaged curve with the mean velocity of each pixel contained in the cross-sectional area for each cardiac phase (bulk quantity) and the other with flow volume estimated in a pixel-wise manner to spatially reflect inhomogeneous flow profile (pixel-wise quantity). The regurgitant fraction (RF, %) was subsequently calculated by BFV relative to FFV, and graded as mild (≤25 %), moderate (25-40 %), and severe (≥40 %).3
Pearson’s correlation coefficient and linear regression model were used to evaluate the bias in RF between bulk and pixel-wise analysis for MPA (n = 16), LPA (n = 26), and RPA (n = 26). Paired t test was also applied to analyze significance of differences between paired variables. Eccentricity at systolic peak (Eccsys) of 0.3 was further adopted as a criterion to categorize RF into 2 groups with spatial flow symmetry and asymmetry.4 Reclassification analysis was performed on RF, showing the amount of cases that changed RF classification after using pixel-wise measurement. The probability value (P) < 0.05 was considered to be statistically significant.
Results
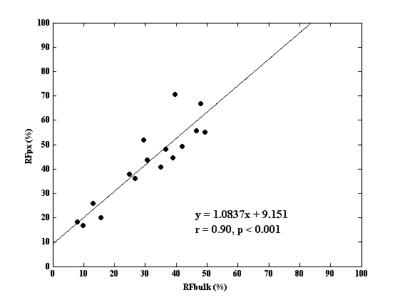
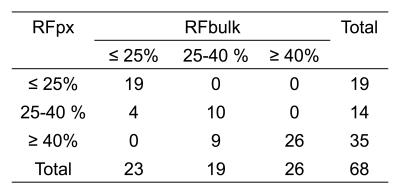
The intercept of the linear regression model in Figure 2 shows that RFbulk was biased by 9.2% in MPA and 15% in LPA (r = 0.95, P<0.001, not shown). The impact of underestimation on RF in RPA (0.8% with r = 0.96, P<0.001, not shown) turns out negligible, associated with differential regurgitation in the branch pulmonary arteries.1 RFbulk are significantly smaller than that of pixel-wise measurement, with mean estimates of 30.9% vs. 42.6%, 42.4% vs. 51.4%, and 31.4% vs. 35.0%, in MPA/LPA/RPA, respectively (P < 0.01). Figure 3 displays further investigation of the RF correlated to flow symmetry during the systolic period. When Eccsys > 0.3, the inconsistency between RFbulk (median: 52%) and RFpx (median: 64%) appears more obvious compared to the other group with Eccsys < 0.3 (median, RFbulk: 30%, RFpx: 38%). This suggests that the RF underestimation using the conventional bulk definition can be more noticeable when severer flow inhomogeneity occurs during the systolic period. Table 1 lists the reclassification of all RF values into three regurgitant severity classes, showing the impact of RF underestimation on clinical diagnosis.Discussion and Conclusion
Our preliminary results demonstrated that 19% of the TOF patients would be reclassified into different regurgitant levels in clinical practice. The quantitative analyses of backward and forward flow volumes in a pixel-wise manner avoid potential cancellation from averaging, and therefore, provide a better indication of the spatial degree of regurgitation. In contrast, RFbulk underestimation was more evident as flow inhomogeneity appeared to increase during the systolic period. In addition, a similar RFbulk can occur in patients with spatial homogeneity and spatial heterogeneity in blood flow profiles, however, the physiologic effects and the implications for treatment might be quite different. A cautious implementation related to flow profile contributes to accuracy of flow quantification; we therefore concluded that the spatial-related flow parameters showed more consistency with the qualitative flow profile pattern for pulmonary arteries and could be a decisive complement for diagnostic classification, especially for patients with marginal moderate RF value.Acknowledgements
No acknowledgement found.References
[1] Gorter, T.M., et al., Pulmonary regurgitant volume is superior to fraction using background-corrected phase contrast MRI in determining the severity of regurgitation in repaired tetralogy of Fallot. Int J Cardiovasc Imaging, 2015. 31(6): p. 1169-77.
[2] Mercer-Rosa, L., et al., Quantifying pulmonary regurgitation and right ventricular function in surgically repaired tetralogy of Fallot: a comparative analysis of echocardiography and magnetic resonance imaging. Circ Cardiovasc Imaging, 2012. 5(5): p. 637-43.
[3] Sigovan, M., et al., Comparison of four-dimensional flow parameters for quantification of flow eccentricity in the ascending aorta. J Magn Reson Imaging, 2011. 34(5): p. 1226-30.
[4] Kang, I.S., et al., Differential regurgitation in branch pulmonary arteries after repair of tetralogy of Fallot: a phase-contrast cine magnetic resonance study. Circulation, 2003. 107(23): p. 2938-43.
Figures