3159
MRI Feature Tracking Strain Provides Incremental Prognostic Information Over Serum Biomarkers in AL Amyloidosis1Radiology, Mayo Clinic, Rochester, MN, United States, 2Cardiovascular Medicine, Mayo Clinic, Rochester, MN, United States, 3Department of Medicine, Division of Hematology, Mayo Clinic, Rochester, MN, United States
Synopsis
The association of MRI feature tracking (FT) strain with all-cause mortality was retrospectively performed on 76 patients with new diagnosis of AL amyloid. Mean follow-up was 4 years. MRI FT radial, circumferential, and longitudinal strain were each associated with all-cause mortality in univariate analysis. In separate multivariate models with serum biomarker stage, radial, circumferential, and longitudinal strain each remained prognostic. This study shows the incremental prognostic value of MRI FT strain in AL amyloidosis.
Introduction
Amyloid light chain (AL) type amyloidosis is a rare systemic disease characterized by tissue deposition of insoluble fibrils made up of plasma cell derived immunoglobulin light chain precursor proteins [1]. Cardiac involvement, found in up to 60% of patients with AL type amyloidosis, is a major determinate of morbidity and mortality [2]. Abnormal myocardial strain as measured with Doppler ultrasound has been found to be prognostic in AL amyloidosis [3]. While magnetic resonance imaging (MRI) strain analysis using myocardial tagging pulse sequences is considered a gold standard for non-invasive strain measurement, there are many practical limitations to this technique, and it is employed infrequently in the clinical setting. Recently, commercial vendors have introduced feature tracking (FT) strain analysis software which can be used with MRI cine balanced steady-state free precession (b-SSFP) images to generate strain values in a method analogous to that used for echocardiographic speckle tracking [4]. However, while several other cardiac MRI parameters have been shown to be prognostic in amyloidosis [5], to date the prognostic significance of MRI FT strain has not been shown amyloidosis. Therefore the purpose of this study was to retrospectively evaluate the prognostic value of MRI FT strain for determining all-cause mortality in AL amyloidosis.Methods:
76 patients with new diagnosis AL amyloidosis underwent cardiac MRI. MRI FT strain analysis was performed on short axis and 3 long axis cine b-SSFP images using commercial software (Circle Cardiovascular Imaging, Inc., Calgary, CA). Endocardial and epicardial borders were manually traced on end-diastolic images with subsequent automatic tracking of the traces through the remainder of the cardiac cycle. Automated traces were visually inspected and manually corrected. In addition, cardiac MRI morphologic and functional evaluation, transthoracic echocardiographic (TTE) diastolic assessment, and serum cardiac biomarker staging were performed. Subjects’ charts were for reviewed for all-cause mortality. Cox proportional hazards analysis was used to evaluate survival in univariate and multivariate analysis.Results:
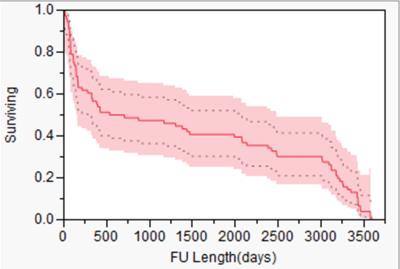
There were 40 deaths, and the median study follow-up period was 4 years (Figure 1). MRI FT radial, circumferential, and longitudinal strain were each associated with all-cause mortality in univariate analysis (hazard ratio (HR) = 0.95, 1.10, and 1.09 respectively for one point change in a strain unit; p < 0.01 for all) (Figure 2). In separate multivariate models with biomarker stage, radial (HR = 0.96, p < 0.01), circumferential (HR = 1.1; p =0.01), and longitudinal strain (HR = 1.07; p = 0.05) each remained prognostic.Discussion:
This study shows the incremental prognostic value of MRI FT strain in AL amyloidosis. MRI FT strain can be included with other MRI parameters to generate prognostic information in AL amyloidosis.Acknowledgements
No acknowledgement found.References
1. Falk RH, Comenzo RL, and Skinner M, The systemic amyloidoses. N Engl J Med, 1997. 337(13): 898-909.
2. Kyle RA and Gertz MA, Primary systemic amyloidosis: clinical and laboratory features in 474 cases. Semin Hematol, 1995. 32(1): 45-59.
3. Barros-Gomes S, Williams B, Nhola LF, Grogan M, Maalouf JF, Dispenzieri A, Pellikka PA, Villarraga HR. Prognosis of Light Chain Amyloidosis With Preserved LVEF: Added Value of 2D Speckle-Tracking Echocardiography to the Current Prognostic Staging System. JACC Cardiovasc Imaging. 2016 (Epub ahead of print)
4. Hor KN, Gottliebson WM, Carson C, Wash E, Cnota J, Fleck R, Wansapura J, Klimeczek P, Al-Khalidi HR, Chung ES, Benson DW, Mazur W. Comparison of magnetic resonance feature tracking for strain calculation with harmonic phase imaging analysis. JACC Cardiovasc Imaging. 2010 Feb;3(2):144-51.
5. Fontana M, Pica S, Reant P, Abdel-Gadir A, Treibel TA, Banypersad SM, Maestrini V, Barcella W, Rosmini S, Bulluck H, Sayed RH, Patel K, Mamhood S, Bucciarelli-Ducci C, Whelan CJ, Herrey AS, Lachmann HJ, Wechalekar AD, Manisty CH, Schelbert EB, Kellman P, Gillmore JD, Hawkins PN, Moon JC. Prognostic Value of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance in Cardiac Amyloidosis. Circulation. 2015 Oct 20;132(16):1570-9.
Figures

Patient Characteristics and Univariate Analyses.
* Indicates a statistically significant difference among the three delayed enhancement patterns without stating which is most associated with prognosis. † Hazard ratios for mass variables are for one gram of mass, one mL/m2 of indexed volume or one percent ejection fraction. ‡ Indicates a statistically significant difference among the three biomarker stages without stating which is most associated with prognosis.. BP = blood pool; CI = confidence interval; HR = hazard ratio; NT-proBNP = N-terminal pro-brain natriuretic peptide; NYHA = New York Heart Association; TTE = transthoracic echocardiography.