3158
Healthy aging of the left ventricle in relationship to cardiovascular risk factors: The Multi-Ethnic Study of Atherosclerosis (MESA)Chia-Ying Liu1, Shenghan Lai2, Nadine Kawel-Boehm3, Harjit Chahal4, Bharath Ambale-Venkatesh4, Joao Lima4, and David Bluemke5
1radiology and imaging sciences, national Institute of Health, bethesda, MD, United States, 2Johns Hopkins School of Medicine, 33Kantonsspital Graubuenden, Clinic of Radiology, 4Johns Hopkins Hospital, 5Radiology and Imaging Sciences, National Institutes of Health
Synopsis
We used cardiovascular magnetic resonance imaging to measure the LV and aortic structure and function in the Multi-Ethnic Study of Atherosclerosis (MESA). The cohort was divided into groups with or without traditional risk factors. In multivariable analyses adjusting for age, sex and race, individuals with risk factors had significantly larger LV mass index (by 17%) and lower LV contractibility (circumference strain, lower by 14%). LV structure and function are also better preserved in senescent hearts in the absence of traditional cardiovascular risk factors.
Introduction
Traditional cardiovascular risk factors are known to accelerate ventricular and vascular aging and either directly or indirectly alter LV structure and function. Their prevalence and extent tends to increase with population aging, thus potentially confounding the independent effects of age in relationship to cardiovascular structure and function. Previous studies that have evaluated the effects of aging on cardiac remodeling have not meticulously excluded subjects with known cardiovascular risk factors. Thus the separate effects and magnitude of advanced age independent of risk factors on cardiovascular structure and function remains unclear. MESA1 examination cohort consists of community-dwelling men and women who had no history of clinical cardiovascular disease at the baseline. Since cardiovascular risk factors are extremely common in the United States, for convenience, we describe individuals without such risk factors as “risk-free”. By characterizing the cardiovascular phenotype of this risk-free population, cardiac function parameters relevant to healthy aging might also be defined to help ascertain risk factor impact on cardiac structure and function.Methods
3015 study participants (48% men, age 55-94, mean 69.01±9.17 years) underwent CMR imaging from 2010-2012. Absence of traditional risk factors (Risk-free: no hypertension, diabetes or impaired fasting glucose, obesity, smoking or hypercholesterolemia) occurred in just 314 (10.4%, 38% men) participants. Differences in the LV/aortic indices between the risk-free and with-risk were studied using unpaired t-test. Age dependence of each CMR measurement was evaluated using univariate linear regression stratified by gender in both groups. To explore the association between LV/aortic indices and risk factors, linear regression was performed with multivariable adjustment for age, sex, race, and risk factors in the entire cohort without dividing into groups.Results
Study subjects without risk factors had a very low incidence of CVD events (2.5%) and myocardial scar (1.9%). Stratified by risk status (Table 1), participants with risk had lower indexed LV volume, larger indexed mass, significantly impaired Ecc, stroke volume index, and descending aortic distensibility, and lower post contrast T1 times compared with risk-free (Figure1). Figure2 shows the effect of age stratified by risk status as well as sex. Indexed LV volumes and stroke volume were inversely associated with age, but such relationships were not statistically significant in risk-free male subjects (p>0.05). Age-associated deterioration in aortic functions remained significant in both genders with or without risk factors. In analyses adjusted for age, sex, and race, obesity, hypertriglyceridemia, hypertension and diabetes were four leading risk factors that affected LV structure and function. Schematic diagrams are plotted in Figure 3 using regression coefficients for the trends of risk status from NO to YES.Discussion
The major differences in LV parameters between participants with or without risks were three fold: with-risk study subjects had greater mass index and smaller cavity volume index, had deteriorated LV contractility, and stroke volume index, and had greater age-associated LV remodeling. Our results support that cardiac structure and function are preserved in senescent hearts without cardiovascular risk factors, and such protection is more prominent in men than in women. Additionally, obesity, hypertriglyceridemia, hypertension, and diabetes denote the major risks of LV structure and function. However, arterial stiffness might be unavoidable in biological aging.Acknowledgements
The authors thank all investigators, staff, and participants of the MESA Study for their valuable contributions. A full list of participating MESA Investigators and institutions can be found at http://www.mesa-nhlbi.org. This research was supported by contracts N01-HC-95159 through N01-HC-95168 from the National Heart, Lung, and Blood Institute.References
1. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr., Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M and Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871-81.Figures

Table 1. Left-ventricular (LV) structure/function and aortic
function of risk-free and with risk MESA participants. Values displayed as
mean±SD (95% confidence interval) and * for p<0.05 between groups after
multivariate adjustment for age/sex/race.
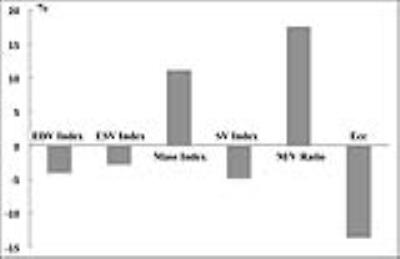
Figure 1. Comparison of LV indices between study subjects with versus
without cardiovascular risk factors.
Percent difference [100×(with-risk – risk-free) ⁄ risk-free] are
shown. All displayed indices are
significantly different between with-risk and risk-free groups.

Figure 2. (A) LV EDV index is
inversely associated with age in all groups. (B) LV mass index in women without
risk factors was independent of age. M/V ratio was positively (C) and stroke
volume index (D) was inversely associated with age but both changes are not
significant in men without risk factors.

Figure 3. Schematic diagrams of
left-ventricular structure and funcion in response to major risk factors.
Regression coefficients from Table 3 were used for the trends of risk status
from NO to YES. For example, LV mass index was higher but stroke volume index
and ejection fraction were lower for smokers (YES) than non-smokers (NO). All correlations displayed are significant
(p<0.05). LV measures without significant correlations to risk factors are
not displayed.