3142
Right ventricular deformation by CMR feature tracking in patients with volume-overload and pressure-overload congenital heart diseases1National Heart Centre Singapore, Singapore, Singapore, 2Duke-NUS Medical School Singapore, Singapore, Singapore
Synopsis
Two major patterns of right ventricular (RV) overload are volume overload and pressure overload. This study aimed to investigate the differences of RV myocardial deformation associated with volume and pressure overload congenital heart diseases. Cardiac magnetic resonance feature tracking was applied to RV 4-chamber and short axis view in a subject group comprising 23 patients with repaired tetralogy of Fallot (rTOF), 23 patients with pulmonary hypertension (PH), and 23 age- and gender-matched normal controls. Results indicated that PH patients had most diminished RV longitudinal and circumferential strain. Patients with rTOF had reduced RV longitudinal strain but higher circumferential strain.
Purpose
The right ventricular (RV) function is one of the most important determinants of mortality and morbidity in patients with congenital heart diseases1. RV volume overload due to pulmonary regurgitation is common in patients with repaired tetralogy of Fallot (rTOF)2. The right ventricle is also exposed to pressure overload by pulmonary stenosis or pulmonary hypertension (PH)1. Current study sought to examine the effect of volume and pressure overload on global RV myocardial deformation by using cardiac magnetic resonance (CMR)-based feature tracking (FT).Methods
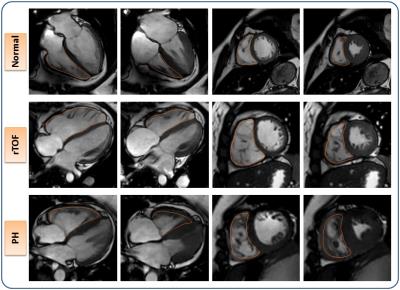
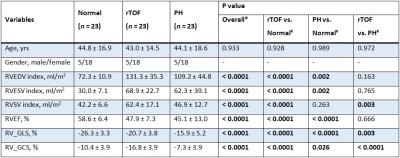
The study population consisted of 23 patients with rTOF (gender male/female 5/18 with age of 43 ± 15 yrs) and 23 patients with PH (gender male/female 5/18 with age of 44 ± 19 yrs). In addition, 23 age- and gender-matched individuals without any cardiovascular disease served as controls (gender male/female 5/18 with age of 45 ± 17 yrs). CMR scan was performed on a 3-Tesla system (Ingenia, Philips Healthcare) using balanced turbo field echo sequences or a 1.5-Tesla system (Siemens Avanto) using steady-state free precession cine gradient echo sequences. End-expiratory breath hold cine images were acquired in multi-planar short- and long-axis views. CMR FT analysis was conducted employing recently introduced QStrain RE software (version 2.0, Medis, Netherlands). The long-axis 4-chamber view was used to derive RV global longitudinal strain (RV_GLS) values. RV global circumferential strain (RV_GCS) measurements were determined in short-axis view at mid-ventricular slice (Fig. 1). For FT analysis, endocardial borders were manually delineated in end-diastolic frame followed by automatic tracking of the endocardial contours by the software throughout the cardiac cycle. Strain results were analyzed using SPSS (version 17.0, Chicago, IL, USA). An F-test was used to test the omnibus hypothesis of equality among patient groups, post hoc Tukey or Games Howell was then performed to test statistically significant difference between each group pair. A P value < 0.05 was regarded statistically significant.Results
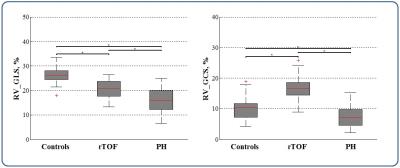
Analysis was feasible for all subjects. RV characteristics were summarized in Table 1. Indexed RV end-diastolic volume (EDV) and end-systolic volume (ESV) were significantly higher in rTOF and PH patients compared to controls (all P < 0.05). RV ejection fraction (EF) was significantly decreased in both patient groups in comparison to controls (all P < 0.0001). The rTOF and PH patients had comparable RVEDV index, RVESV index and RVEF (all P > 0.05). On FT, RV global longitudinal strain (RV_GLS) values were significantly reduced in both rTOF (-20.7 ± 3.8% vs. -26.3 ± 3.3%, P < 0.0001) and PH patient groups (-15.9 ± 5.2% vs. -26.3 ± 3.3%, P < 0.0001) compared to the control group. Patients with PH had significantly smaller RV_GLS than rTOF patients (P = 0.003). The values of RV_GLS were strongly correlated with RVEF (r = -0.693, P < 0.0001). Interestingly, RV global circumferential strain (RV_GCS) was significantly higher in patients with rTOF when compared with normal controls (-16.8 ± 3.9% vs. -10.4 ± 3.9%, P < 0.0001), while patients with PH had significantly reduced RV_GCS values compared to both rTOF patients and healthy subjects (also see Fig. 2).Discussion
Global RV longitudinal strain from long-axis 4-chamber view and circumferential strain from short-axis were considered in current study due to their high level of reproducibility3. Circumferential RV strain was found to be larger in rTOF patients compared to controls, which was in agreement with earlier study4. The reason for increased circumferential strain was unclear. Kempny et al.4 indicated that the circumferential strain may be underestimated in control subjects due to more pronounced out of plane motion. However, we think this phenomenon is likely related to increased transverse shortening in compensation for the loss of systolic function of the RV outflow tract (RVOT) in rTOF patients with preserved RVEF5,6.Conclusions
Current study examined RV deformation in patients with volume overload and pressure overload congenital heart diseases. PH patients had most impaired RV longitudinal and circumferential strain compared to rTOF patients and controls. The patients with rTOF had reduced RV longitudinal strain but increased circumferential strain in comparison with normal controls.Acknowledgements
No acknowledgement found.References
1. Voelkel NF, Quaife RA, Leinwand LA, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114(17):1883-1891.
2. Maskatia SA, Spinner JA, Morris SA, et al. Effect of branch pulmonary artery stenosis on right ventricular volume overload in patients with tetralogy of fallot after initial surgical repair. Am J Cardiol. 2013;111(9):1355-1360.
3. Padiyath A, Gribben P, Abraham JR, et al. Echocardiography and cardiac magnetic resonance-based feature tracking in the assessment of myocardial mechanics in tetralogy of Fallot: an intermodality comparison. Echocardiography. 2013;30(2):203-210.
4. Kempny A, Fernández-Jiménez R, Orwat S, et al. Quantification of biventricular myocardial function using cardiac magnetic resonance feature tracking, endocardial border delineation and echocardiographic speckle tracking in patients with repaired tetralogy of Fallot and healthy controls. J Cardiovasc Magn Reson. 2012;14:32.
5. Greutmann M, Tobler D, Biaggi P, et al. Echocardiography for assessment of regional and global right ventricular systolic function in adults with repaired tetralogy of Fallot. Int J Cardiol. 2012;157:53-58.
6. Koestenberger M, Ravekes W, Nagel B, et al. Reference values of the right ventricular outflow tract systolic excursion in 711 healthy children and calculation of z-score values. Eur Heart J Cardiovasc Imaging. 2014;15:980-986.
Figures