3133
Evaluating Circle of Willis using Simultaneous Non-Contrast Angiography and intraPlaque Hemorrhage (SNAP)1Chongqing Medical University, Chongqing, People's Republic of China, 2Department of Biomedical Engineering, School of Medicine, Tsinghua University, 3Departement of Biomedical Engineering, School of medicine, Tsinghua University, Beijing, People's Republic of China
Synopsis
The purpose of this study is to evaluate the ability of SNAP to evaluate the CoW by comparing with an established non-contrast MRA technique, time of flight (TOF).We found SNAP have good agreement with TOF and similar intra-reader reproducibility in CoW evaluation. However, the agreement between TOF and SNAP and the reproducibility of each technique is moderate in the anterior communicating artery identification. Thus, SNAP shows great promise for imaging both intracranial artery and vessel wall with a single scan.
Purpose
As the major intracranial collateral circulation pathway,
circle of Willis (CoW) has attracted significant attention because its status
may affects the occurrence and outcome of stroke1-3. Recently, Simultaneous
Non-contrast Angiography and intraPlaque hemorrhage (SNAP) technique was proposed,
which can be used as a non-contrast MRA technique4, 5. Although SNAP has been investigated in intracranial arteries 4, its ability to evaluate CoW has not been validated in
any literature. In this study, we sought to evaluate the ability of SNAP
to evaluate the CoW by comparing with an established non-contrast MRA
technique, time of flight (TOF).Methods
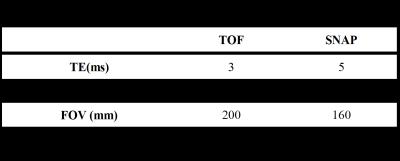
Population: After written informed consent was obtained, 53 patients (30 males, mean age=57±7.8 years) with ischemic stroke occurred within 3 months were recruited. MR imaging: All subjects were scanned on a Philips 3T scanner with a 32-channel head coil. The MR imaging protocol included TOF and SNAP. The imaging parameters are detailed in Table 1. Data analysis: All post-processing and review was done using a Philips workstation. First, non-contrast MRAs were generated using Maximal Intensity Projection for TOF and Minimal Intensity Projection for SNAP. Then, an experienced radiologist reviewed the TOF and SNAP MRAs blindly to the patient information to evaluate the presence/absence of the constituent vessels of CoW, including the A1 segments of anterior cerebral arteries (ACAs), anterior communicating artery (A-comA), P1 segments of posterior cerebral arteries (PCAs) and posterior communicating arteries (P-comAs). To test the intra-reader reproducibility, all images were reviewed again 2-week after the first review to avoid memory bias. The vessel is determined as 'present' if the start and end points of a vessel are present on the MRA image6. Then the CoW can be defined as complete CoW (all constituent arteries are present) and incomplete CoW (some constituent arteries are absent).The Cohen's Kappa was used to evaluate the reproducibility and compare the SNAP MRA and TOF MRA in evaluating CoW.Results
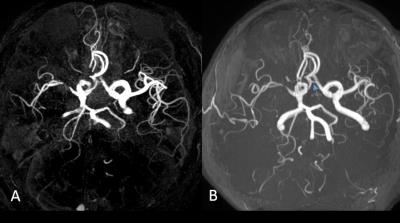
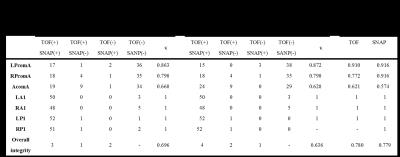
Comparisons of the CoW artery presence in SNAP and TOF, and comparison between the first and the repeated review are shown in Table 2. The intra-reader reproducibility of SNAP and TOF in CoW evaluation were similar, they all showed good to excellent reproducibility in LPcomA, RPComA, LA1, RA1, LP1 and RP1 and the overall integrity evaluation. The reproducibility in evaluating AcomA were lower for both SNAP and TOF. In evaluating CoW, SNAP showed a good to excellent agreement with TOF, especially in LPcomA, RPComA, LA1, RA1, LP1 and RP1, the agreement in evaluating AcomA was lower, but still acceptable. Fig 1 shows an example case where the AcomA is obvious on TOF but hard to see on SNAP.Discussion
The results of this
study prove the feasibility of SNAP in CoW evaluation. Performance of SNAP and
TOF are similar in depicting most of the arterial segments of CoW. The reproducibility
of SNAP in most segments of CoW is also very good. Although SNAP has lower
agreement with TOF on AcomA, the κ value is
similar to the reproducibility of TOF and SNAP on AcomA identification,
indicating identification of AcomA segment is poor for both SNAP and TOF. This
may be caused by the small diameter of AcomA. To improve the performance of
AcomA identification, contrast-enhanced MRA technique could be used.Conclusion
This study proved that SNAP has the ability to evaluating the integrity of CoW, further extending the ability of SNAP to be used as a non-contrast MRA technique, as well as vessel wall evaluation tool.Acknowledgements
None.References
1. Chuang Y-M, Chan L, Lai Y-J, et al. Configuration of the circle of Willis is associated with less symptomatic intracerebral hemorrhage in ischemic stroke patients treated with intravenous thrombolysis. J Crit Care. 2013;28(2):166-172.
2. Zeng J, Fan Y. Correlation Between the Integrity of the Circle of Willis and the Severity of Initial Noncardiac Cerebral Infarction and Clinical Prognosis. 2016;95(10):1-7.
3. Paper O. Absent Collateral Function of the Circle of Willis as Risk Factor for Ischemic Stroke. 2003:191-198.
4. Wang J, Guan M, Yamada K, et al. In Vivo Validation of Simultaneous Non- Contrast Angiography and intraPlaque Hemorrhage ( SNAP ) Magnetic Resonance Angiography?: An Intracranial Artery Study. 2016:1-10.
5. Wang J, Börnert P, Zhao H, et al. Simultaneous noncontrast angiography and intraplaque hemorrhage (SNAP) imaging for carotid atherosclerotic disease evaluation. MagnReson Med. 2013; 69(2):337–345.
6. Krabbe-Hartkamp MJ, van der Grond J, de Leeuw FE, et al. Circle of Willis: morphological variation on MR angiograms. Radiology.1998;207:103–111.
Figures