3130
Velocity-selective unenhanced peripheral MR angiography: Initial clinical testing compared with digital subtraction angiography1Diagnostic Radiology and Nuclear Medicine, University of Maryland, Baltimore, MD, United States, 2New York University, New York, NY, United States, 3Vascular Surgery, University of Maryland, Baltimore, MD, United States, 4Cardiovascular Medicine, Case Western Reserve, Cleveland, OH, United States
Synopsis
We performed initial clinical testing of velocity-selective magnetization-prepared MR angiography (VS-MRA) in 31 patients with peripheral arterial disease with digital subtraction angiography (DSA) serving as the reference standard. The image quality score of VS-MRA was 2.8±0.6 in the scale of 0-3 (0: non-diagnostic, 3: excellent). The sensitivity and specificity for detecting significant stenosis were 90.1 % and 96.2%, respectively on a per-segment basis (n=286), and were 92.7% and 92.0 %, respectively on a per-region basis (n=105). The Fleiss-Cohen κ value for the agreement between VS-MRA and DSA was 0.91 on a per-segment basis and 0.88 on a per-region basis.
Purpose
Velocity-selective (VS) magnetization-prepared imaging is a new unenhanced MR angiography (MRA) method, which generates angiographic contrast by suppressing stationary tissues while highlighting fast-moving arterial blood based on their velocities. VS-MRA has shown great promise for abdominal, peripheral and cerebral territories in limited number of healthy subjects1-3. The purpose of this study is to evaluate image quality and diagnostic performance of VS-MRA in patients with peripheral arterial disease (PAD) with digital subtraction angiography (DSA) serving as the reference standard.Methods
Thirty one patients were prospectively recruited among those who were visiting the University of Maryland Vascular Clinic due to known or suspected PAD (mean age = 60.9, 22 men). While all the 31 participants underwent unenhanced VS-MRA, 24 of them (mean age = 59.8, 17 men) underwent clinical DSA examinations 1 - 67 days (mean = 19 days) later than the MR examinations with no vascular intervention taking place between the MR and DSA studies.
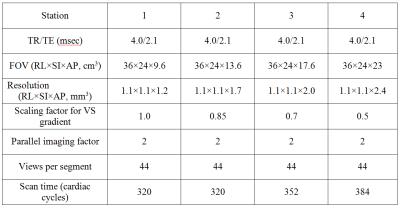
Unenhanced VS-MRA was performed on a Siemens 1.5 T clinical MR scanner (Siemens Medical Solutions, Erlangen, Germany). Four stations (numbered 1 for the most inferior level) were used for a superior-to-inferior coverage of 4×24 = 96 cm with the imaging parameters summarized in Table 1. Velocity-selective MRA pulse sequence was electrocardiographically triggered, and consisted of a 90° VS saturation preparation pulse, a fat saturation pulse and a segmented 3D balanced SSFP acquisition in each cardiac cycle. The VS saturation preparation pulse consisted of five RF hard pulses for excitation and four 90x-180y-90x composite pulses for refocusing, interleaved with a series of unipolar gradients for velocity encoding2.
The image quality of VS-MRA images was assessed on consensus by a cardiologist and a vascular surgeon on a four-point scale (0- non-diagnostic, 1- fair, 2-good, 3- excellent) after dividing the arterial tree into common iliac, external iliac, common femoral, superficial femoral, popliteal, tibiofibular trunk, anterior tibial, posterior tibial, and peroneal arteries. The stenosis severity was evaluated on both MR angiograms and DSA images, based on a 4-point scale: 0-normal, 1-less than 50% stenosis, 2-greater than 50% stenosis, 3- occlusion. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy of VS-MRA were calculated for determination of nonsignificant (<50%) versus significant (50%-100%) stenosis and also for determination of occlusion, with DSA as the reference standard. All the diagnostic measures were calculated on per-segment, and per-region bases. Agreement between NCE MRA and DSA regarding stenosis classification was evaluated per segment and region by using the Fleiss-Cohen quadratic weighted κ statistics.
Results
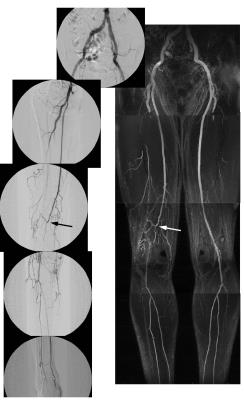
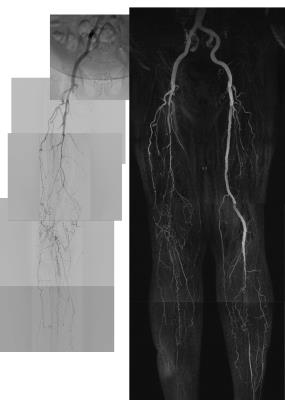
Figures 1-3 illustrate representative VS-MRA and DSA images in three patients. For 530 arterial segments available in VS-MRA, the image quality score was excellent with a mean of 2.8 (in the scale of 0-3) and a standard deviation of 0.6. Five segments (0.9%) were rated as non-diagnostic (score 0), and their anatomical locations were iliac artery (n=2), femoral artery (n=3) and posterior tibial artery (n=1). All the five non-diagnostic segments involved arterial signal loss presumably due to B1 field inhomogeneity which distorts VS excitation profile.
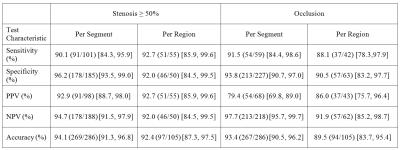
Two hundreds eighty six arterial segments were available in both DSA and MRA images and were used for diagnostic testing. The sensitivity and specificity of VS-MRA for detecting significant stenosis (≥50%) were 90.1% and 96.2%, respectively when calculated on a per-segment basis (n=286), and were 92.7% and 92.0 % when calculated on a per-region basis (n=105). The sensitivity and specificity for detecting occluded segments were 91.5% and 93.8%, respectively on a per-segment basis and were 88.1% and 90.5% on a per-region basis. Other diagnostic measurements are summarized in Table 2.
Velocity-selective MRA showed excellent concordance with DSA in classifying the degree of stenosis on both per-segment and per-region bases, as represented by κ of 0.91 and 0.88, respectively. The stenosis grading of VS-MRA was concordant with DSA in 79.4% of segments (227/286) with underestimation in 11.2% of segments (32/286) and overestimation in 9.4% of segments (27/286). In 5.9% (17/286), the disagreement was clinically significant (in assessing whether or not there was stenosis >50% or occlusion).
Discussion
We have shown that unenhanced VS-MRA enables clear delineation of the entire peripheral arterial tree and accurate assessment of stenosis, as evidenced by high diagnostic agreement with DSA. Velocity-selective MRA has advantages of high spatial resolution in all 3 dimensions (unlike inflow-based 2D multi-slice approaches4) and need for single acquisition only (as opposed to subtractive 3D approaches5,6). While this initial clinical study shows the potential of the VS-MRA technique as a safe and accurate tool for the evaluation of PAD, comparisons with other MRA methods and CTA are warranted.Acknowledgements
This work was supported by R21EB019206.
References
1. Shin T, Worters PW, Hu BS, Nishimura DG. Non-contrast-enhanced renal and abdominal MR angiography using velocity-selective inversion preparation. Magn Reson Med. 2013;69:1268-1275
2. Shin T, Hu BS, Nishimura DG. Off-resonance-robust velocity-selective magnetization preparation for non-contrast-enhanced peripheral mr angiography. Magn Reson Med. 2013;70:1229-1240
3. Qin Q, Shin T, Schar M, Guo H, Chen H, Qiao Y. Velocity-selective magnetization-prepared non-contrast-enhanced cerebral mr angiography at 3t. Magn Reson Med. 2015;75:1232-1241
4. Edelman RR, Sheehan JJ, Dunkle E, Schindler N, Carr J, Koktzoglou I. Quiescent-interval single-shot unenhanced magnetic resonance angiography of peripheral vascular disease: Technical considerations and clinical feasibility. Magn Reson Med. 2010;63:951-958
5. Fan Z, Sheehan J, Bi X, Liu X, Carr J, Li D. 3d noncontrast mr angiography of the distal lower extremities using flow-sensitive dephasing (fsd)-prepared balanced ssfp. Magn Reson Med. 2009;62:1523-1532
6. Priest AN, Graves MJ, Lomas DJ. Non-contrast-enhanced vascular magnetic resonance imaging using flow-dependent preparation with subtraction. Magn Reson Med. 2012;67:628-637
Figures