3128
The value of 3T contrast-enhanced whole-heart Coronary MRA in a integrated assessment of Cardiac Magnetic Resonance Protocol for Detection of suspected or known Coronary Artery Disease1Radiology Department, Beijing Anzhen Hospital, Capital Medical University, Beijing, People's Republic of China, 2Cedars-Sinai Medical Center, Biomedical Imaging Research Institute,University of California, Los Angeles, United States
Synopsis
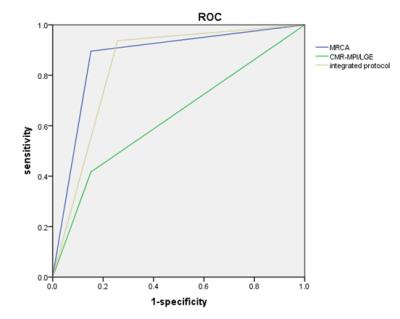
We try to evaluate the additive diagnostic value of a 3T whole-heart CE-MRCA integration into a CMR-MPI/LGE protocol for the detection of coronary artery disease A total of 38 subjects were examined by CMR (including CMR-MPI, MRCA, and LGE)[j1] and x-ray invasive coronary angiography (ICA). Diagnostic performances of MRCA, CMR-MPI/LGE, and MRCA+CMR-MPI/LGE integration were determined having XA as standard for coronary artery disease. In per-vessel analysis, integrated protocol (AUC=0.84) performed better than the isolated CMR-MPI/LGE (AUC=0.63). In this suspected or known coronary artery disease population, integration of CE-MRCA significantly improved per-vessel diagnostic accuracy of a comprehensive 3T CMR-MPI/LGE protocol.
Introduction/Purpose
First-pass myocardial MR perfusion(MPI) has become a reliable tool for the diagnosis of myocardial ischemia. Contrast-enhanced magnetic resonance coronary angiography (CE-MRCA) has been shown to be able to show the lesion and anatomy of the coronary artery, but its incremental value as part of a CMR protocol including MPI and late gadolinium enhancement (LGE) is not well established. The purpose of this study was to evaluate the additive diagnostic value of a 3-dimensional whole-heart CE-MRCA integration into a 3T CMR-MPI/LGE protocol for the coronary artery disease.Method
Thirty-eight symptomatic patients (54.7±11.5 years; 74% men) with suspected or known coronary artery disease underwent CMR (including CMR-MPI, MRCA, and LGE) and x-ray invasive coronary angiography (ICA). CMR was performed on a 3.0T whole-body scanner (MAGNETOM Verio, Siemens Healthcare, Erlangen, Germany). A 32-element cardiac matrix coil was activated for data collection. For perfusion imaging, 3 short-axis slices (basal, midventricular, and apical) were acquired under maximal hyperemia achieved with 140 μg・kg−1・min−1 IV ATP infusion, during the first pass of a bolus of 0.05 mmol・kg−1 of gadolinium injected at 5 mL・s−1 through a dedicated right antecubital vein. Cine scans were performed between stress and rest perfusion acquisitions with a balanced SSFP sequence. A navigator-gated, ECG-triggered, fat-saturated, inversion-recovery prepared segmented 3D FLASH sequence was employed for whole heart coronary MRA with additional infusion of contrast medium (0.1mmol/kg at 2ml/s). LGE images were collected by phase sensitive inversion recovery sequence .The total acquisition time is 56.8min.Result
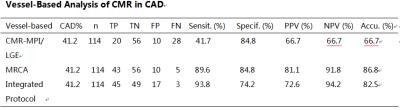
Diagnostic performances of MRCA, CMR-MPI/LGE, and MRCA+CMR-MPI/LGE integration were determined having XA as standard for coronary artery disease (≥50% stenosis/occlusion in vessels>2 mm). In per-vessel analysis, integrated protocol (AUC=0.84) performed better than the isolated CMR-MPI/LGE (AUC=0.63) and similarly to the isolated MRCA(AUC=0.87). In per-vessel analysis, MRCA had 90% sensitivity, 85% specificity, 81% positive predictive value and 92% negative predictive value. CMR-MPI/LGE had 42% sensitivity, 85% specificity, 67% positive predictive value and 67% negative predictive value. Integration of MRCA with CMR-MPI/LGE further improved CMR performance to 94% sensitivity, 74% specificity, positive predictive value of 72%, and negative predictive value of 94%, with a global accuracy of 82%. On per-segment analysis, MRCA shows right coronary artery and left anterior descending branch well, but poorly for The distal segment of left circumflex branch and left circumflex branch.Discussion/Conclusion
In this suspected or known Coronary Artery Disease population, integration of contrast-enhanced whole-heart MRCA significantly improved per-vessel diagnostic accuracy of a comprehensive 3-T stress-rest CMR-MPI/LGE protocol.
The use of 3T CE-MRCA integration into a CMR-MPI/LGE was not seen in the previous literature. In this study, we try to examine whether 3T CE-MRCA can improve the diagnostic efficacy of coronary heart disease. But the data is not large enough, so for the per-patient analysisis is not accurate enough.
Acknowledgements
Thanks for all people in our study.References
1. Bettencourt N, Ferreira N, Chiribiri A,et al. Additive value of magnetic resonance coronary angiography in a comprehensive cardiacmagnetic resonance stress-rest protocol for detection of functionally significant coronary artery disease: a pilot study.Circ Cardiovasc Imaging. 2013 Sep;6(5):730-8.
2. Pereira E, Bettencourt N, Ferreira N,et al. Incremental value of adenosine stress cardiac magnetic resonance in coronary artery disease detection. Int J Cardiol. 2013 Oct 9;168(4):4160-7.
3.Qi Yang, Kuncheng Li, Xin Liu,et al.Contrast-Enhanced hole-Heart Coronary MRA at 3.0T: A Comparative Study with X-ray Angiography in a Single Center. J Am Coll Cardiol. 2009 June 30; 54(1): 69–76.
Figures
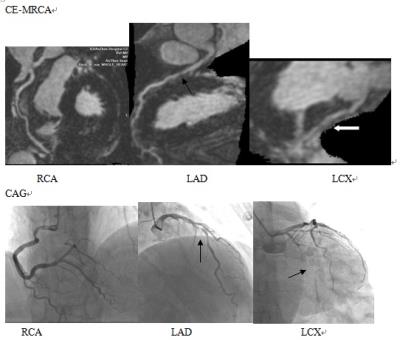
CE-MRCA and CAG, men, 63-year-old,CAG displayed LCX Occlusion and LAD Severe stenosis.CE- MRCA correctly identified significant stenoses .
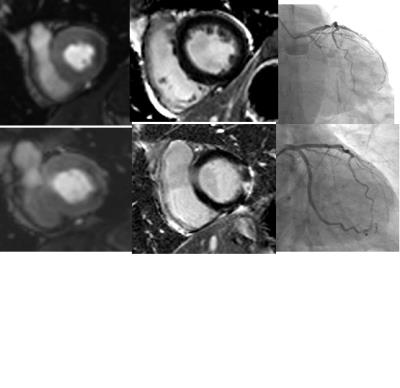
The three pictures above : CMR stress perfusion show Left ventricular lateral wall myocardial ischemia.
The three pictures below: After 45 days, the same patient referred for CMR and CAG for recurrent chest pain. LGE show lateral wall infarction. CAG show distal stent in LCX occlusion.