3099
Simultaneous Imaging of Myocardial Fat and Scar using Dark Blood Late Gadolinium Enhancement1Division of Imaging Sciences and Biomedical Engineering, King's College London, London, United Kingdom, 2Department of Medicine, Beth Israel Deaconess Medical Centre and Harvard Medical School, Boston, MA, United States
Synopsis
Dark-Blood Late Gadolinium Enhancement (DB-LGE) sequence has been recently introduced to suppress the blood signal in order to enhance the contrast between blood and scar. However, it is difficult to distinguish scar from fat as both appear bright in DB-LGE images. In this study, we present a DB-LGE sequence that allows quantification of scar and fat volume in the heart in a single imaging sequence. Numerical simulation, phantom and in-vivo scans were performed to evaluate the proposed sequence.
Background
Dark-Blood Late Gadolinium Enhancement (DB-LGE) sequence, based on a combination of T2 magnetization preparation and inversion pulse, has been recently introduced to suppress the blood signal in order to enhance the contrast between blood and scar [1]. A short T1 time of fat causes the fat signal to recover rapidly, therefore scar and fat will appear with high signal value which makes it difficult to distinguish scar from fat. Furthermore, quantification of fat has both diagnostic and prognostic value. In this study, we sought to develop a DB-LGE sequence that allows quantification of scar and fat volume in the heart in a single imaging sequence.Methods
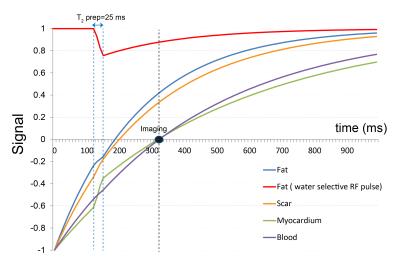
The DB-LGE sequence uses an optimized combination of the inversion and T2 preparation in order to suppress both healthy myocardium and blood signal based on the higher T2 value of the blood [1]. In this study, we propose to develop a sequence (Fig. 1) for simultaneous scar and fat imaging. Thus,we implemented a dual-echo gradient echo data acquisition in DB-LGE sequence to allow for water and fat separation using two-point Dixon reconstruction [2]. Furthermore, in order to increase the signal-to-noise ratio of the fat signal to improve robustness of Dixon reconstruction, we implemented a water selective inversion preparation pulse (WS INV) (Fig. 1). WS INV pulse inverts the magnetization of water, but the fat signal will not be disturbed and remains high. Contrast-scout sequence was used to determine the proper Δt1, Δt2 and Δt3 to null both normal myocardium and blood immediately before acquiring images [1]. Numerical simulation experiment was performed to investigate the signal of blood, fat, myocardium and scar in the presence of the DB-LGE sequence, with and without WS INV pulse. To evaluate the proposed sequence, with and without water selective preparation pulse a phantom experiment was performed using nine NiCl2-doped agarose vials with different T1/T2 values (416/21, 1083/43, 454/188 (blood), 547/42(myocardium), 1358/45, 1551/238, 290/41, 793/44, 250/153ms) and a bottle of oil. Two vials of the phantom represent the post contrast myocardium and blood. Scans were performed on a 1.5T Philips Achieva scanner equipped with a 32-element cardiac coil with the following imaging parameters: TR/TE1/TE2=7.4/2.1/5.1ms, flip angle=25˚, FOV=310×310mm2, voxel size=2×2mm2, slice thickness=8mm and acquisition time=9 second. In-vivo images were also acquired in patients undergoing clinical cardiac MR. To track the respiratory motion, a respiratory navigator was positioned on the right hemi-diaphragm.Results
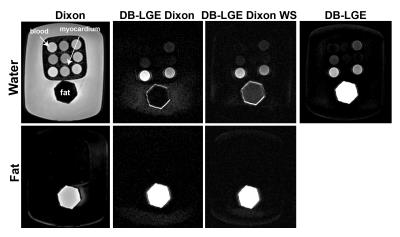
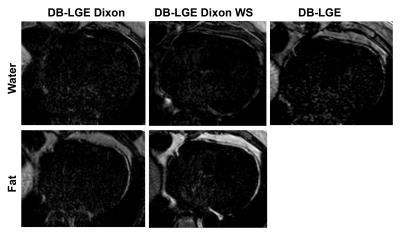
Fig. 2 shows that by using the WS INV pulse, there is significant increase in fat signal. In the phantom study, the appropriate parameters to null both the normal myocardium and blood were Δt1/Δt2 /Δt3=285/25/95ms. Fig. 3 shows the fat and water images with Dixon, DB-LGE with Dixon, DB-LGE with Dixon and WS INV, and the conventional DB-LGE images. By using the WS INV the SNR of fat signal in the fat image is increased (DB-LGE with Dixon: SNRfat=65.5, DB-LGE with Dixon and WS INV: SNRfat= 108.5). Fig. 4 shows the DB-LGE images and corresponding fat image that were acquired in a patient with cardiomyopathy.Conclusion and Discussion
The proposed imaging sequence allows simultaneous imaging of scar tissue and fat signal. Application of a water-selective inversion pulse improved signal from fat which could improve the robustness of the Dixon reconstruction. Further studies in patients with myocardial infarction and myocardial fat are needed to thoroughly evaluate the proposed sequence.Acknowledgements
This work was supported by EPSRC grants EP/P001009/1 and EP/P007619/1, and FONDECYT N°1161051.References
[1] Basha T, Rojoul S, Kissinger et al. Black blood late gadolinium enhancement using combined T2 magnetization preparation and inversion recovery. JCMR 17(Suppl 1):O14.
[2] Dixon WT. Simple proton spectroscopic imaging. Radiology 1984;153(1):189-194.
Figures