3098
Improved Detection of Right Ventricular Myocardial Infarction Using 3D Navigator-Gated Free Breathing Delayed Enhancement Cardiac Magnetic Resonance1Department of Cardiology, Weill Cornell Medical College, New York, NY, United States, 2Department of Medicine, Weill Cornell Medical College, New York, NY, United States, 3Department of Radiology, Weill Cornell Medical College, New York, NY, United States
Synopsis
Right ventricular myocardial infarction (RV-MI) is a serious consequence of coronary artery disease that adversely affects outcomes. Conventional CMR employs 2D breath-held imaging (CMRBH) to detect RV-MI, an approach that may sacrifice spatial resolution to enable patient breath-holds, and is thus suboptimal for imaging the RV. This study compared 3D navigator-gated free breathing CMR (CMRNAV) to CMRBH for detection of RV-MI in 75 post-MI patients. Results demonstrated a 2-fold increase in detection rate of RV-MI by CMRNAV, accompanied by higher spatial resolution in 30% less scan time.
Purpose
Right ventricular myocardial infarction (RV-MI) impacts clinical outcomes, increasing risk of adverse cardiac events by almost three-fold, and affects therapeutic decision-making for patients with coronary artery disease.1 Inversion recovery cardiac magnetic resonance (CMR) is well validated for assessment of left ventricular MI,2 but conventional serial 2D breath-held methods often have limited spatial resolution or coverage due to slice gap or misregistration between consecutive slices, and is thus suboptimal for imaging the thin-walled RV.3 3D navigator gated free breathing CMR (CMRNAV) has been shown to be clinically efficient and to provide high spatial resolution imaging for detection of LV MI,4,5 but this pulse sequence has not been tested for RV-MI. This study compared free breathing CMRNAV to the conventional approach of 2D breath-held imaging (CMRBH) for detection of RV-MI among a broad cohort of at-risk post-MI patients.Methods
The population comprised a consecutive research cohort of post ST segment elevation MI patients at risk for RV-MI secondary to right coronary artery occlusion. All patients underwent a standardized protocol at 1.5T [GE], inclusive of attempted post-contrast inversion recovery imaging via both CMRBH and CMRNAV. For CMRBH, a commercially available 2D breath-held pulse sequence was employed (typical TR/TE/FA/rBW = 7.0 ms/3.4 ms/20°/±15.63 kHz, matrix=256x192, 24 views per segment, 2 R-R intervals, slice thickness 6mm, inter-slice gap 4mm). For CMRNAV, a 3D free-breathing pulse sequence was developed that combines partial k-space acquisition with the efficient 2-bin phase-ordered automatic window selection real-time diaphragmatic navigator-gating algorithm (typical TR/TE/FA/rBW=4.8 ms/1.5 ms/20°/±62.5 kHz, matrix=256x256, 36 views per segment, thickness 5 mm, no gap, 4mm gating window).4 Both CMRBH and CMRNAV were acquired in contiguous short axis slices, extending from RV outflow tract through the apex. Delayed enhancement images generated by each pulse sequence were read independently by blinded expert physicians for presence of RV-MI, which was defined in accordance with standard criteria as discrete hyperenhancement in RV wall myocardium. Signal (SNR) and contrast-to-noise (CNR) ratios were measured in reader-assigned regions of RV-MI. Ancillary analysis was used to assess markers of RV-MI, including adjacent LV-MI burden as well as quantitative indices of RV and LV structure/function (measured via SSFP cine-CMR).Results
75 post-MI patients (58±13 yo, 87% male) underwent CMR within 6 weeks (4±1 weeks) of index MI; 32% (n=24) had RV-MI identified by either CMRBH or CMRNAV. Both CMRBH and CMRNAV were acquired in 91% of patients (8% navigator failure, 1% breath-hold intolerance). In-plane spatial resolution was higher via CMRNAV vs. CMRBH (x-orientation: 1.4±0.1 vs. 1.4±0.1 mm, p=0.09½ y-orientation: 1.2±0.2 vs. 1.4±0.2 mm, p<0.01) and voxel size was smaller (8.6±2.2 vs. 19.8±3.7 mm3, p<0.01) as was primarily attributed to improved z-axis coverage (5mm contiguous slice thickness vs. 6mm with 4mm inter-slice gap). Higher spatial resolution was provided by CMRNAV in 30% less acquisition time on average for cumulative data acquisition (276±169 vs. 394±145 sec, p=0.002). The diaphragmatic navigator efficiency was 42±15%. RV-MI prevalence was 2-fold higher via CMRNAV vs. CMRBH (32% vs. 16%, p<0.001) (Figure 1). All patients with RV-MI on CMRBH were detected by free breathing CMRNAV. Among patients with RV-MI detected by both techniques, quantitative assessment demonstrated 17.2% higher SNR (p=0.03) and 8.7% higher CNR (p=0.001) for RV-MI detected by CMRNAV as compared to CMRBH (Figure 2). CMRNAV incrementally detected RV-MI in patients with lesser RV injury, as evidenced by greater RV chamber dilation (162±40ml vs. 129±35ml, p=0.045) and a trend towards lower RVEF (56±8 vs. 61±7; p=0.08) among patients with RV-MI detected by both techniques as compared to those detected by CMRNAV alone.Discussion
Conventional segmented delayed enhancement CMR for RV-MI is limited by visualization of contrast-enhancement in the thin RV myocardium; this limitation has contributed to varying incidence of RV-MI in prior literature.3,6.7 Our findings illustrate that CMR technique strongly impacts RV-MI detection whereby free-breathing 3D navigator CMR results in a 2-fold increase in RV-MI detection in 30% less scan time as compared to standard 2D breath-held CMR. Of note, scan success rate of 92% in this study was slightly better than that reported in prior patient studies using 3D navigator technique for other structures including the coronaries.8 Future studies are warranted to further optimize CMRNAV sequence utilizing parallel imaging or improved motion tracking9 at 3T field strength, towards the goal of accelerated 3D imaging for RV-MI.Conclusion
3D CMRNAV inversion recovery imaging yields a 2-fold increase in RV-MI detection rate with 30% less acquisition time compared to conventional assessment via 2D CMRBH. Improved RV-MI detection via CMRNAV is attributable to higher spatial resolution, and is accompanied by parallel increases in both CNR and SNR.Acknowledgements
No acknowledgement found.References
1. Miszalski-Jamka T1, Klimeczek P, Tomala M, Krupinski M, Zawadowski G, Noelting J, Lada M, Sip K, Banys R, Mazur W, Kereiakes DJ, Zmudka K, Pasowicz M. Extent of RV dysfunction and myocardial infarction assessed by CMR are independent outcome predictors early after STEMI treated with primary angioplasty. JACC CV Imaging. 2010; 3:1236-46.
2. Simonetti OP, Kim RJ, Fieno DS, Hillenbrand HB, Wu E, Bundy JM, Finn JP, Judd RM. An improved MR imaging technique for the visualization of myocardial infarction. Radiology. 2001;218:215-23.
3. Kumar A, Abdel-Aty H, Kriedemann I, Schulz-Menger J, Gross CM, Dietz R, Friedrich MG. Contrast-enhanced cardiovascular magnetic resonance imaging of right ventricular infarction. JACC CV Imaging 2006; 48:1969-76.
4. Nguyen TD, Spincemaille P, Weinsaft JW, Ho BY, Cham MD, Prince MR, Wang Y. A fast navigator-gated 3D sequence for delayed enhancement MRI of the myocardium: comparison with breathhold 2D imaging. J Magn Reson Imaging. 2008;27:802-8.
5. Pierce IT, Keegan J, Drivas P, Gatehouse PD, Firmin DN. Free-breathing 3D late gadolinium enhancement imaging of the left ventricle using a stack of spirals at 3T. J Magn Reson Imaging. 2015;41:1030-7.
6. Grothoff M, Elpert C, Hoffmann J, Zachrau J, Lehmkuhl L, de Waha S, Desch S, Eitel I, Mende M, Thiele H, Gutberlet M. Right ventricular injury in ST-elevation myocardial infarction: risk stratification by visualization of wall motion, edema, and delayed-enhancement cardiac magnetic resonance. Circ Cardiovasc Imaging. 2012;5:60-8.
7. Masci PG, Francone M, Desmet W, Ganame J, Todiere G, Donato R, Siciliano V, Carbone I, Mangia M, Strata E, Catalano C, Lombardi M, Agati L, Janssens S, Bogaert J. Right ventricular ischemic injury in patients with acute ST segment elevation myocardial infarction: characterization with cardiovascular magnetic resonance. Circulation. 2010;122:1405-12.
8. Dewey M, Teige F, Schnapauff D, Laule M, Borges AC, Wernecke KD, Schink T, Baumann G, Rutsch W, Rogalla P, Taupitz M, Hamm B. Noninvasive detection of coronary artery stenoses with multislice computed tomography or magnetic resonance imaging. Ann Intern Med. 2006 Sep 19;145(6):407-15.
9. Henningsson M, Prieto C, Chiribiri A, Vaillant G, Razavi R, Botnar RM. Whole-heart coronary MRA with 3D affine motion correction using 3D image-based navigation. Magn Reson Med. 2014;71:173-81.
Figures
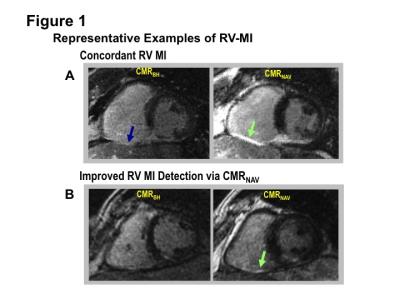
Figure 1:
Representative examples of RV-MI.
A. Typical examples of concordant RV-MI detection by CMRBH (blue arrow) and CMRNAV (green arrow). Note extension of LV inferior wall infarction into the RV inferior wall as is typical for RV involvement in LV inferior wall MI.
B. Improved
RV-MI detection via CMRNAV. CMRNAV demonstrates regional
hyperenhancement in RV inferior wall (green arrow) not evident on CMRBH
(images shown in matched spatial location).
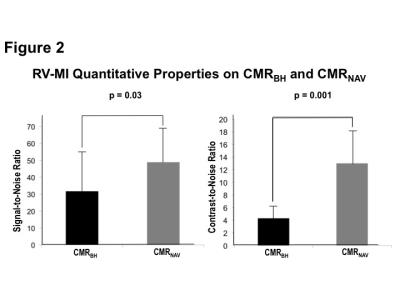
Figure 2:
SNR (left) and CNR (right) within RV-MI concordantly identified by CMRBH and CMRNAV (data shown as mean ± standard deviation). Note higher CNR and SNR for RV-MI detected by CMRNAV as compared to CMRBH (p<0.05 for both).