3095
Reducing magnetization-transfer-induced T1 estimation error in myocardial T1 mapping for the MOLLI sequence: simulation, phantom and in vivo studies1Radiology, University of California, Los Angeles, CA, United States, 2Division of Cardiology, University of California, Los Angeles, CA, United States
Synopsis
The modified Look-Locker inversion-recovery (MOLLI) sequence is a widely used myocardial T1 mapping technique for tissue characterization. It is known that the MOLLI sequence underestimates myocardial T1 values (>10%) due to magnetization transfer (MT) effects and short myocardial tissue T2 values. In this work, we demonstrate that in vivo reduction of the inversion factor is predominantly responsible for the MT effect that reduces MOLLI T1 values. Thus, using an alternative T1 estimation algorithm with a measured inversion factor for the MOLLI sequence can reduce the MT effect on T1 estimation error.
Background
Myocardial T1 mapping is an emerging technique used to assess diffuse myocardial fibrosis. Among various myocardial T1 mapping techniques, the modified Look-Locker inversion-recovery (MOLLI) sequence (1) has good precision and reproducibility but is less accurate. Conversely, while SASHA (2) has good accuracy, it is less precise. A recent study showed that together, effects from T2 relaxation and magnetization transfer (MT)-induced reduction of T1 are responsible for > 15% myocardial T1 underestimation as measured by MOLLI (3). In this work, we will demonstrate that a reduction in the inversion factor due to in vivo MT effects is the predominant reason for MT’s effect on MOLLI derived T1 values. In this proof-of-concept study, we use data from simulations, phantoms, and in vivo studies to support an alternative T1 estimation algorithm with a measured inversion factor for the MOLLI sequence as a possible solution for reducing MT effect on T1 estimation error.Methods
The MOLLI pulse sequence was studied on a 1.5T scanner (Avanto Fit, Siemens Healthcare, Erlangen, Germany). In this work, we applied a previous technique, BLESSPC (Bloch equation simulation with slice profile correction) (4), which was originally proposed for spoiled gradient echo readout, to bSSFP-based MOLLI acquisitions. By assuming a fixed T2 = 45 ms, the modified BLESSPC remains a suitable fit with three free parameters (T1, M0, flip angle FA) or four free parameters (T1, M0, FA and inversion factor δ). The “MOLLI+M0” sequence, which acquires an additional proton density weighted image without an inversion pulse 3s following the MOLLI 3(3)3(3)5 acquisition, was implemented for measurement of δ.
T1 estimation using the MOLLI 5(3)3 sequence and the inversion factor estimation using the “MOLLI+M0” sequence was evaluated using simulation, phantoms and in vivo studies. To evaluate the influence of MT on measured inversion factor and T1 estimations, the “MOLLI+M0” sequence and the MOLLI 5(3)3 sequence were simulated at heart rate (HR) = 60 bpm without and with MT. The simulated tissue parameters were the same as that of cardiac muscle used in (3). The “MOLLI+M0” and MOLLI 5(3)3 images were acquired on nine gel phantoms (2%-4% agar) at simulated HR = 60 bpm and on eight healthy volunteers.
BLESSPC four-parameter fitting was applied to the “MOLLI+M0” data to estimate inversion factors. BLESSPC three-parameter fitting was applied to MOLLI 5(3)3 to calculate T1 values using a fixed δ from 0.88 – 1.00 (0.01 increment) in simulations. The measured average δ was used in phantoms and in vivo studies, respectively. For comparison, the T1 values were also calculated using the original MOLLI fitting based on the same data.
Results
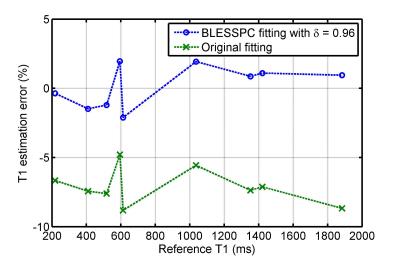
The average inversion factor δ measured on 9 phantoms was 0.96±0.01, which is close to the estimated δ value (0.97) based on the simulated non-MT “MOLLI+M0” data. The average δ measured on native myocardial tissues in vivo was 0.88±0.01, which is close to the estimated value (0.89) when MT effects were simulated. Therefore, MT is the major reason for the reduced inversion factor in vivo compared to observations in phantom experiments. As shown in Figure 1, the original fitting will result in >10% additional T1 estimation error due to MT effects. In comparison, using BLESSPC fitting with a measured δ reduced the T1 estimation error to less than 1% in both scenarios similar to phantom (no MT) and in vivo (with MT).
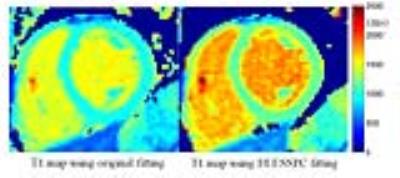
In phantom studies, using BLESSPC fitting with δ = 0.96 reduced the absolute T1 estimation error to 1.3%±0.6% from 7.1%±1.3% (original fitting) for the MOLLI sequence (Figure 2). The average native myocardial T1 value using BLESSPC fitting with δ = 0.88 was 1151.3±22.7 ms, which is close to the previously reported values (1170 ± 9 ms) using the SASHA technique, a method that is less sensitive to MT effects (3). In comparison, the original fit resulted in significantly lower myocardial T1 values (964.4±19.7 ms, relative T1 difference = -16.2%±0.5%, p < 0.001). The T1 estimation difference between the original and BLESSPC fitting in phantoms and in vivo studies agreed well with the simulation results (without MT and with MT effects). Figure 3 shows an example of the myocardial T1 maps generated using the original fitting and BLESSPC fitting for the MOLLI data acquired in a healthy volunteer.
Conclusion
The measured in vivo inversion factor was much lower than the phantom inversion factor due to MT effects. BLESSPC fitting can be used for the MOLLI sequence to reduce the T1 estimation error, including errors due to MT effects.Acknowledgements
N/AReferences
1. Messroghli DR, Greiser A, Fröhlich M, Dietz R, Schulz-Menger J. Optimization and validation of a fully-integrated pulse sequence for modified look-locker inversion-recovery (MOLLI) T1 mapping of the heart. J. Magn. Reson. Imaging 2007;26:1081–6.
2. Chow K, Flewitt JA, Green JD, Pagano JJ, Friedrich MG, Thompson RB. Saturation recovery single-shot acquisition (SASHA) for myocardial T(1) mapping. Magn. Reson. Med. 2014;71:2082–95.
3. Robson MD, Piechnik SK, Tunnicliffe EM, Neubauer S. T1 measurements in the human myocardium: the effects of magnetization transfer on the SASHA and MOLLI sequences. Magn. Reson. Med. 2013;70:664–70.
4. Shao J, Rapacchi S, Nguyen K-L, Hu P. Myocardial T1 mapping at 3.0 tesla using an inversion recovery spoiled gradient echo readout and bloch equation simulation with slice profile correction (BLESSPC) T1 estimation algorithm. J. Magn. Reson. Imaging 2016;43:414–25.
Figures