Mehrdad Pourfathi1, Yi Xin1, Maurizio Cereda2, Stephen Kadlecek1, Harrilla Profka1, Hooman Hamedani1, Ian Duncan1, Sarmad Siddiqui1, Nicholas Drachman1, Kai Ruppert1, and Rahim Rizi1
1Radiology, University of Pennsylvania, Philadelphia, PA, United States, 2Anesthesiology and Critical Care, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
In
this study, hyperpolarized [1-13C]-pyruvate imaging
was used to investigate the effect of positive-end expiratory pressure (PEEP) on the stabilization of lung
metabolism after injury. Results demonstrated significantly lower lactate-to-pyruvate ratio in rats ventilated with PEEP.
Introduction
Ventilator induced lung injury (VILI)
results from mechanical trauma and secondary inflammatory responses. Protective
ventilation and positive-end expiratory pressure (PEEP) can attenuate cytokine
concentrations and inflammatory infiltrates due to atelectasis (atelectrauma),
protecting the lungs from the progression of pre-existing lung inflammation
[1,2]. Previous metabolic imaging studies have focused on how glucose uptake is
affected by ventilator settings. In this study, the conversion of hyperpolarized
[1-13C]-pyruvate to [1-13C]-lactate was used to
investigate the effect of PEEP on the stabilization of lung metabolism after
injury. Methods
Seven
Sprague-Dawley rats (341±38g) were ventilated with a tidal volume (TV) of 8.1±0.8
mL/kg and PEEP of 7±2cmH2O (protective ventilation) for t=60min, followed
by tracheal hydrochloric acid (pH 1.25, 1.0mL/kg) instillation at t=70min. These
ventilation settings were maintained until t=120min. PEEP was then lowered to
zero in four rats and kept stable until the end of the experiment (t=300min) in
three rats. Dynamic pulmonary compliance was calculated in the absence of PEEP by
dividing peak inspiratory pressure measured via pressure meter by the TV
delivered to the rat, and was used to monitor injury progression [3]. Rats were
imaged in supine position using a 1H/13C quadrature
birdcage coil (m2m) at 4.7T (Varian Inc.). Proton images were acquired using a
multi-slice gradient-echo sequence (TR/TE=80/1.5ms, α=10°, 128x128 voxels). Hyperpolarized
[1-13C]-pyruvate imaging was conducted at t=60min (baseline), t=120min
(follow-up 1), and t=300min (follow-up 2). ~22 µL of [1-13C]-pyruvate
was polarized using a HyperSense DNP polarizer to over 25%. The sample was
melted using 4mL of a dissolution buffer (40mM Trizma, 160mM NaOH, 50mM NaCl,
0.1g/L EDTA) at 180°C to yield a neutralized isotonic solution of 80mM [1-13C]-pyruvate
at ~37°C. 12 seconds after dissolution, 4ml/kg of the hyperpolarized agent was administered
via the tail-vein over 6s. A single-slice axial carbon-13 chemical shift image
was acquired using a 16x16 FID-CSI sequence (TR/TE=35/0.35ms, α=12°), with a
custom outward spiral k-space trajectory [4]. Imaging started 12 seconds after
the end of injection (in-plane FOV=45x45mm2, 15mm slice thickness). A
12s breath-hold was applied to minimize the respiratory motion artifact during
carbon imaging. Blood oxygen level was monitored using a pulse oximeter during
the scan. The peaks in the phase-corrected real part of the spectra was fit to
Lorentizan functions and metabolites
were quantified by finding the area under the fits using custom-made routines in
MATLAB2014b. Processed carbon images were converted to DICOM format and overlaid
on the proton image using OsiriX 8.0.Results and Discussion
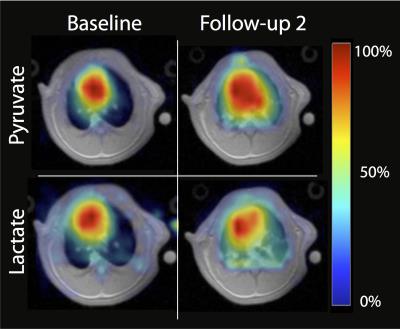
Figure 1 shows pyruvate and lactate maps overlaid on
proton images before and four hours after instillation of HCl in a rat
ventilated with no PEEP. The intensity of each image is normalized to its own
maximum intensity. The images show increased pyruvate and lactate signal post-injury.
The increased pyruvate signal was likely due to increased capillary permeability,
while the enhanced lactate signal was chiefly caused by an inflammatory
response to the acute injury characterized by neutrophilic infiltration in the
lungs [5-6]. Figure 2 shows the
average lactate-to-pyruvate (top) and pulmonary compliance (bottom) measured for
each group at three different time points. Average lactate-to-pyruvate ratio increased
by 16% in rats ventilated with PEEP between hours 2 and 5. However, this ratio
increased by 76% in the rats ventilated with no PEEP (p<0.05). The observed effect size (Cohen’s d) for this
measurement was 1.67. Rats ventilated without PEEP had a significant decline of
compliance at the 5-hour time point compared with the rats ventilated with PEEP
(p<0.01), indicating lung injury progression and atelectasis.Conclusions
This study used hyperpolarized [1-13C]-pyruvate
imaging to investigate differences in metabolism of injured lungs after protective
and non-protective ventilation. The significant increase observed in the
lactate-to-pyruvate ratio is due to the recruitment of neutrophils caused by
atelectrauma and by over-distention of the ventilated alveoli leading to VILI
[5-6]. Increased progression of lung
injury in rats ventilated with no PEEP is confirmed by the significant decline in
pulmonary compliance at the 5-hour time point compared to rats ventilated with
PEEP. This study shows that in the presence of pre-existing lung injury, hyperpolarized
carbon-13 MRI can detect secondary inflammation in the absence of PEEP by
measuring changes in cellularity and bioenergetics of the lungs. This
information is critical for early detection and management of lung injury.Acknowledgements
This work was
supported by the National of Institutes of Health (NIH) R01 HL124986.References
[1] Pinhu, et al. Lancet. 361:332–40 (2003). [2]
Tremblay et al. J. Clinical Investigations. 99(5):944-952 (1997). [3] Cereda M,
et al. Anesthesiology 2016;124:121–131. [4] Kadlececk S, et al. The 24th Annual
Meeting of ISMRM 2016. [5] KENNEDY TP, et al. anesth. Analg. 1989;69:87–92. [6] Shaghaghi et. al., NMR in biomedicine,
27(8):939-947 (2014).