2922
MRI Efficacy Evaluation of AvastinTM in Combination Temozolomide Therapy using GL261 Tumor Bearing Mice1Laboratory Animal Center, Osong Medical Innovation Foundation, Cheongju, Korea, Republic of
Synopsis
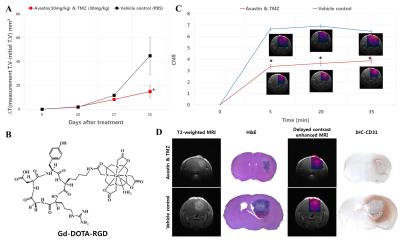
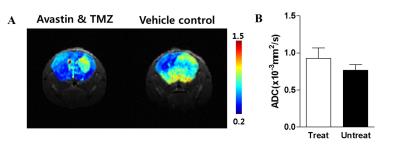
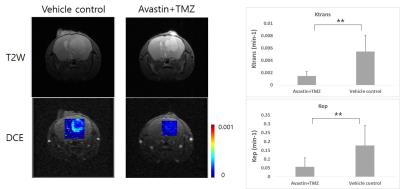
The aim of this study was to evaluate of the drug efficacy used by MRI. A mouse were randomly divided into the control and therapy groups for treatment. MRI were performed to compare with two groups and significant differences were observed in the two groups. The volume transfer constant (Ktrans), flux rate constant (kep) and contrast agent (Gd-DOTA-RGD) enhancement were decreased in the therapy group. Apparent diffusion coefficient (ADC) was lower in the control group. Furthermore, histopathologic assessments were in accord with MRI. Based on these results, efficacy evaluation used by MRI can be helped the development of new bio-drug.
Introduction
New drug discovery is a relatively long process. Many imaging techniques have been routinely used in the drug discovery process to directly monitor the drug treatment in the context of disease. MRI has been successful in the pharmaceutical industry for the evaluation of preclinical drug efficacy and clinical trials. It is a non-invasive imaging technique with superb sort tissue contrast capable of delivering quantitative 3D information on organ anatomy and function. Because it is non-invasive aside from the need to anaesthetize animals to immobilize them during image acquisition, animals can be imaged on multiple occasions and studies can be designed so that each animal serves as its own control increasing the statistical power of experiments and allowing group sizes to be reduced. However, despite penetration into preclinical and clinical drug efficacy studies, there are relatively few reports of the use of MRI in drug efficacy studies. Therefore, this study aims to evaluate the efficacy of bio and chemical drug used by MRI in GL261 brain tumor bearing mice.Methods
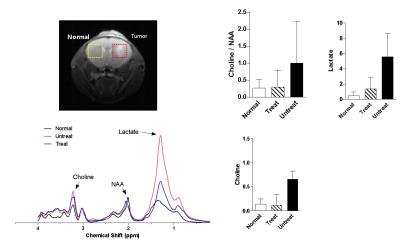
The mouse glioblastoma cells were cultured in RPMI 1640 medium with L-Glutamine (Corning) containing 1% (v/v) penicillin and 10% (v/v) fetal bovine serum at 37°C in a 5% CO2 incubator. Injection into the right cerebral hemisphere of GL261 cells suspended in PBS (1ⅹ105/mouse) was performed using a 4 μL micro-syringe under mechanical control to avoid brain injuries during the procedure. A total of 18 mouse GL261 tumor-bearing C57BL/6 mice were randomly divided into the combined treatment of Avastin (10 mg/kg) and temozolomide (TMZ, 30 mg/kg) and control groups for treatment with an intraperitoneal injection.1 The mice were observed for 21 days and the tumor growth and MRI of the mice in the two groups were analyzed. For MRI studies, therapy effects were monitored using a Bruker 4.7 T (Bruker, Ettlingen, Germany). Delayed contrast-enhanced MRI using an axial T1-weighted, spin echo sequence with the following parameters: TR=800msec, TE=10msec, average=30, matrix=128ⅹ96, slice thickness=1mm. The total examination time was obtained by bolus tail vein injection with Gd-DOTA-RGD2 (0.2 mmol/kg) for 50 minutes. We also performed diffusion weighted image (DWI): TR=2000msec, TE=30msec, average=3, matrix=96ⅹ96, FOV=20ⅹ20, slice thickness=1mm, and magnetic resonance spectroscopy (MRS): TR=2500msec, TE=17msec, average=256, voxel size=3ⅹ3ⅹ3mm3, scan time=10min 40sec, dynamic contrast-enhanced MRI (DCE-MRI): TR=20msec, TE=2.38msec, flip angle=30o, repetition=600, matrix=128ⅹ128, FOV=20ⅹ20, slice thickness=1mm, scan time=1h 4min 18sec. After 21 days GL261 cells injection, the brains were removed and embedded with paraffin, cut into consecutive 6 μm sections. The sections were stained with haematoxylin-eosin (H&E), and endothelial immunohistochemistry (IHC) stain of angiogenesis using CD31 and observed vascular density and structural changes under the microscope.3Results
After Avastin and TMZ therapy, brain tumor volume decreased at days 10, 17, 21 after initiation of injection as compared with controls, but differences did reach statistical significance at day 21 (Figure 1A).4 Combined therapy resulted in significantly decreased CNR (Gd-DOTA-RGD, 0.2 mmol/kg) at all observed time points after 21 days injection of drug as compared with controls (Figure 1B and 1C). Histology analysis in control animals revealed larger vessels area than therapy group. Furthermore, H&E and IHC assessments were in accord with T2 weighted and delayed contrast-enhanced MRI (Figure 1D). ADC values in animals treated with Avastin and TMZ were higher than those of controls after 21 day, no statistically significant differences between the groups were observed (Figure 2B). Control group, compared to therapy group NAA (N-acetyl-aspartate) have fallen and cho (choline) and Lac (lactate) has increased (Figure 3). Values for kep and ktrans were significantly decreased in animals after treatment than in untreated mice at day 21 (Figure 4)Conclusions
The aim of the present study was to evaluate the efficacy of bio and chemical drug used by MRI in a mouse brain tumor model. We observed that bio-drug and chemotherapy significantly decreased the vascular density of the tumor tissue by MRI and histologic assessments. In front of, bio-drug combined with chemotherapy has a good application prospect in the treatment of cancer. The therapy effect of the combinational strategy is significant and the combined treatments makes the approach worthy of clinical application. Therefore, efficacy evaluation used by MRI can be helped the development of this.Acknowledgements
No acknowledgement found.References
1. Siemann D W, Shi W, et al. Dual Targeting of Tumor Vasculature: Combining Avastin and Vascular Disrupting Agents (CA4P or OXi4503). Anticancer Res. 2008;28:2027-2032.
2. Park JA, Lee JJ, Jung JC, Yu DY, Oh C, Ha S, Kim TJ, Chang Y, et al. Gd-DOTA Conjugate of RGD as a Potential Tumor-Targeting MRI Contrast Agent. ChemBioChem. 2008;9:2811-2813.
3. Muldoon LL, Gahramanov S, Li X, Marshall DJ, Kraemer DF, Neuwelt EA, et al. Dynamic magnetic resonance imaging assessment of vascular targeting agent effects in rat intracerebral tumor models. Neuro Oncol. 2011;13(1):51-60.
4. Oh B, Han J, Choi E, Tan X, Lee M, et al. Peptide Micelle-Mediated Delivery of Tissue-Specific Suicide Gene and Combined Therapy with Avastin in a Glioblastoma Model. Journal of pharmaceutical sciences. 2015;104:1461-1469.
Figures