2915
Reproducibility of Quantitative DW-MRI and DCE-MRI of the Breast in the Community Setting: Preliminary Results1Internal Medicine, University of Texas at Austin, Austin, TX, United States, 2Biomedical Engineering, University of Texas at Austin, Austin, TX, United States, 3Institute for Computational Engineering and Sciences, University of Texas at Austin, Austin, TX, United States, 4Neuroscience, University of Texas at Austin, Austin, TX, United States, 5US Oncology Network, Austin, TX, United States, 6Seton Medical Center, Austin, TX, United States, 7Austin Radiological Association, Austin, TX, United States
Synopsis
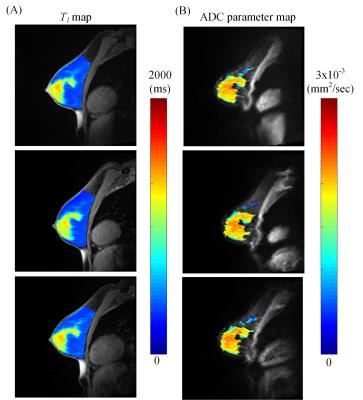
Implementation of quantitative DCE-MRI and DW-MRI in the community setting has the potential to impact patient care for a large number of breast cancer patients. Quantitative DW-MRI and DCE-MRI was assessed in phantoms and normal subjects across three sites. In normal subject fibroglandular tissue, the average percent difference in ADC across sites for all subjects was 1.8%, while the average percent difference in the inversion recovery scan and B1- corrected T1 map were 14% and 7.3%, respectively. Overall, the results from the phantom and normal subject scans reveal that quantitative MRI can be successfully implemented in the community setting.
Purpose
This study assessed implementation and reproducibility of quantitative dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DW-MRI) of the breast in the community setting. Accurate and early response assessment to neoadjuvant therapy (NAT) would provide the opportunity to replace an ineffective treatment with an alternative regimen, potentially avoiding/curtailing side effects. Quantitative MRI has been shown to predict breast tumor response to treatment early during the course of NAT.1 Importantly, integrating quantitative imaging techniques into the community-based setting has the potential to reach a large percentage of breast cancer patients. This study evaluated the ability to implement and assess the reproducibility of T1 mapping (for quantitative DCE-MRI analysis) and ADC mapping (from DW-MRI data) in the community setting through evaluations of both phantom studies and normal human subjects.Methods
Imaging data from phantoms and normal subjects were acquired at two community imaging facilities and one research facility using 3T Siemens Skyra scanners equipped with an 8- or 16-channel receive double-breast coil (Sentinelle, Invivo). To investigate the feasibility of the T1-mapping approaches, eight gel phantoms (The Eurospin II Test System, Diagnostic Sonar) submerged in water were scanned at room temperature (T1 values ranged from 300 to 1600 ms). A coronal image volume was placed in the center of the breast coil containing the phantoms. A multiple flip angle (MFA) approach was implemented with 10 flip angles (2, 4, 6, …, 20) using a three-dimensional spoiled gradient echo (SPGE) sequence with the following parameters: TR/TE = 7.9/2.71 ms and a GRAPPA acceleration factor of 3. As a gold standard, a two-dimensional inversion recovery (IR) prepared turbo-spin echo (TSE) sequence was used to acquire a single slice corresponding to the center of the variable flip angle image with 10 inversion times (50, 75, 100, 200, 300, 400, 500, 1000, 2000 and 4000 ms). An ice-water diffusion phantom2 was also scanned at each of the locations with an echo-planar monopolar spin-echo with the following parameters: TR/TE: 3000/52 ms, diagonal b-values of 0, 200, 800 s/mm2, and GRAPPA acceleration factor of 2. DW-MRI data was used to extract apparent diffusion coefficient (ADC) values for every voxel. Normal subjects (N=2) were scanned at each of the facilities in the sagittal plane using the aforementioned sequences and imaging parameters. Fibroglandular tissue (FGT) from each breast was segmented using the IR images, and the mean T1 and ADC was calculated. Signal to noise ratios and percent error were calculated to assess reproducibility of T1 and ADC mapping between community imaging sites. Percent difference between T1 mapping techniques was also quantified.Phantom Results
For the DW-MRI studies, the ADC values within the phantom averaged 1.25 x 10-3 mm2/sec ± 0.07 x 10-3 mm2/sec. The average percent difference was 6.8% between any two sites. For T1 mapping, the phantom revealed an average percent difference of 6.1% in the inversion recovery sequence between the sites. There was discrepancy between the T1 maps from the multi-flip angle map with the B1 correction and the IR sequence; in the phantom there was a 17.5% average percent difference when comparing the two maps.Volunteer Results
For
the DW-MRI studies in normal subjects, the ADC values of the FGT revealed an
average percent difference of 1.1% and 2.7% for subject 1 and 2, respectively,
between the various sites. For T1
mapping using the inversion recovery sequence, the normal subjects revealed an
average percent difference of 9.0% and 1.4% error between the sites. Additionally,
reproducibility between the sites revealed a 3.7% and 10.7% average percent
difference in normal subjects for the B1-
corrected T1 mapping of
FGT. In comparing the two T1 mapping approaches in the
normal subject FGT, there was an average percent difference of 8.3% across
sites.Discussion
Overall, the results from the phantom and normal subject scans reveal that quantitative MRI of the breast can be implemented in the community setting, and that these measurements may be useful for assessing breast tumors. Additionally, the reproducibility between sites was encouraging, although additional work needs to be completed using a B1-corrected T1 map in this setting. We are currently acquiring additional data on healthy volunteers in preparation for performing a proper reproducibility analysis. Quantitative DW-MRI and DCE-MRI have potential to greatly improve the accuracy of prediction of response in breast tumors when evaluating response to NAT.Conclusion
Quantitative DCE-MRI and DW-MRI can be implemented in the community-based imaging setting. A recently opened clinical trial is currently using these protocols to predict the response of breast tumors to NAT in the community setting.Acknowledgements
We thank the National Cancer Institute for support through U01CA174706 and U01CA142565. We thank the Cancer Prevention and Research Institute of Texas (CPRIT) for funding through RR160005. T.E.Y. is a CPRIT Scholar of Cancer Research.References
1. Li X, Kang H, Arlinghaus LR, et al. Analyzing spatial heterogeneity in DCE- and DW-MRI Parametric Maps to Optimize Prediction of Pathologic Response to Neoadjuvant Chemotherapy in Breast Cancer. Trans Oncology. 2014; 7(1):14-22.
2. Chenevert TL, Galban CJ, Ivancevix MK, et al. Diffusion coefficient measurement using a temperature controlled fluid for quality control in multi-center studies. J Magn Reson Imaging. 2011; 34(4):938-987.
Figures