2882
Cardiovascular Magnetic Resonance (CMR) imaging quantification of right and left ventricular strain in repaired Tetralogy of Fallot: Preliminary results in 10 patients and 10 normal volunteers1Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Patients with repaired Tetralogy of Fallot (rTOF) have worsening right and left ventricular function due to their lack of a functional pulmonary valve and the resulting pulmonary insufficiency. Determining the severity of this dysfunction is important for deciding when interventions like pulmonary valve replacement become necessary. Radial and longitudinal myocardial strain is a functional parameter than can aid in this clinical decision. In this small study, myocardial strain was calculated using tissue tracking software applied to axial cine balanced steady-state free precession (bSSFP) images. Significant differences in RV and LV radial and longitudinal strain were found between patients with rTOF and healthy volunteers.
PURPOSE:
To quantify radial and longitudinal strain of the right and left ventricle in patients with repaired Tetralogy of Fallot (rTOF) and compare those values to those found in normal volunteers. We used tissue tracking software applied to CMR sequences in the axial plane to determine if there were significant differences in these parameters between these two groups.METHODS:
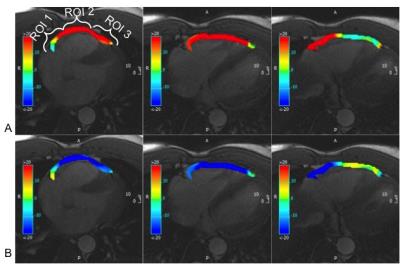
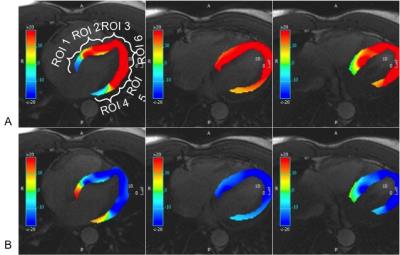
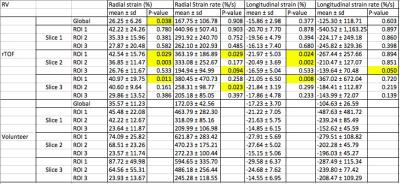
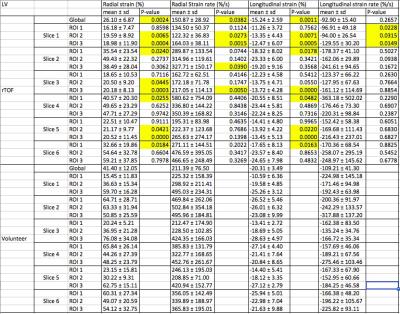
In this IRB approved retrospective study radial and longitudinal strain and strain rates were quantified in 10 patients with repaired Tetralogy of Fallot (rTOF) and 10 healthy volunteers. These were derived from the bSSFP axial images using tissue-tracking software (cmr42, Circle Cardiovascular Imaging, Inc., Calgary, Canada) (Figures 1 and 2). Strain values were measured for the right ventricle (RV) and left ventricle (LV) using contours drawn on three contiguous mid ventricle axial planes. The RV free wall was divided into three regions of interest (ROIs): the basal (ROI 1), mid (ROI 2) and apical (ROI 3) segments of the RV free wall. The LV was divided into six ROIs with similar basal, mid and apical divisions along the interventricular septum and LV free wall. Differences in strain and strain rates between the two groups were made using un-paired t-tests. A p value of < 0.05 was used to determine statistical significance.RESULTS:
In the RV, the global radial strain in the rTOF patients was significantly lower than in the healthy volunteers (26.3 ± 6.3% vs. 35.6 ± 11.3%, p=0.04). ( Tables 1 and 2).The RV global longitudinal strain values were not significantly different (-16.2 ± 3.0% vs. -17.2 ± 3.7%, p=0.37). Both LV global radial and longitudinal strain were of lower magnitude in the rTOF patients compared to healthy volunteers (26.1 ± 6.9% vs. 41.4 ± 11.3%, p=0.002) and (-15.2 ± 2.6% vs. -20.3 ± 3.2%, p=0.001), respectively. No significant difference was seen for the radial and longitudinal strain rates. The values of global radial and longitudinal strain obtained in the healthy volunteers agree with those found in the literature [1].DISCUSSION:
Almost all patients with rTOF will inevitably suffer from progressive RV and LV dysfunction that may ultimately require pulmonary valve replacement (PVR). Clinically it is often difficult to determine when PVR is necessary. These decisions are often based on physiologic parameters like worsening pulmonary regurgitation, decreasing RV and LV ejection fractions and increasing indexed end diastolic volumes that can be measured on CMR[2]. Strain measurements can also be used to assess ventricular dysfunction and may be useful in deciding when it is time to intervene on patients with rTOF. Strain is typically assessed with echocardiography, but cardiac MRI is being used more frequently for these measurements[3, 4]. Our results indicate that the simple technique employed in our study is promising for evaluating myocardial strain and using it to assess the severity of RV and LV dysfunction in patients with rTOF. This study is not without limitations. The population of rTOF patients used in this study is heterogeneous due to differences in age, type of repair and time since repair. The small sample size also limits the generalizability of the results.CONCLUSION:
This preliminary study shows that CMR is a viable modality for quantifying myocardial strain to evaluate the degree of RV and LV dysfunction in patients with rTOF. This technique requires no additional CMR sequences and minimal additional post- processing. The significance of these results and their agreement with values from the literature suggests that further investigation of this method may be complementary to currently used indices for stratifying patients with rTOF and determining when it is time to intervene.Acknowledgements
We wish to acknowledge research support to the Department of Radiology from GE Healthcare.References
1. Dohi K, Sugiura E, Ito M. Utility of strain-echocardiography in current clinical practice. Journal of echocardiography. 2016;14(2):61-70.
2. Geva T. Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. Journal of cardiovascular magnetic resonance : o?cial journal of the Society for Cardiovascular Magnetic Resonance. 2011;13:9.
3. Toro KD, Soriano BD, Buddhe S. Right ventricular global longitudinal strain in repaired tetralogy of Fallot. Echocardiography. 2016;33(10):1557-62.
4. Gursu HA, Varan B, Sade E, Erdogan I, Ozkan M. Analysis of right ventricle function with strain imaging before and after pulmonary valve replacement. Cardiology journal. 2016;23(2):195-201.
Figures