2881
Application of optimized TPAT technique in evaluating arrythmia patients' cardiac function1Beijing Anzhen Hospital, Beijing, People's Republic of China, 2Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, People's Republic of China, 3MR Collaborations NE Asia, Siemens Healthcare, Beijing, China
Synopsis
Traditional CMR sequences are useful tools for assessing cardiac structure and function, However, the poor image quality and motion artifacts caused by arrhythmia may hamper the diagnostic quality of CMR images. We hypothesized that the optimized temporal parallel acquisition technique (TPAT) may improve this situation by allowing free-breathing of subjects and meanwhile provides a similar diagnostic values for radiologists .
Purpose
Traditional CMR sequences are useful tools for assessing cardiac structure and function, However, the poor image quality and motion artifacts caused by arrhythmia may hamper the diagnostic quality of CMR images. We hypothesized that the optimized temporal parallel acquisition technique (TPAT) may improve this situation by allowing free-breathing of subjects and meanwhile provides a similar diagnostic values for radiologists.Methods
Experiment: Thirteen patients with arrhythmia and 13 patients with normal heart rhythm were were included in this study. CMR scan was performed using a 3.0T system (MAGNETON Verio, Siemens Healthcare, Erlangen, Germany). Cine images were acquired by bSSFP sequence with conventional retrospective ECG-triggering method and the optimized real-time TPAT technique in the same planes. The optimized TPAT sequence allows for free-breathing scans, which is beneficial for those with a poor breath-hold. Parameters of the conventional scan including: voxel size 1.3×1.3×5.0mm3, TR/TE 41.1/1.51ms, FOV 340×289 mm2, scan time per slice 12 s, temporal resolution 41.1ms; The parameters of TPAT scan were: voxel size 2.9×2.1×8.0mm3, TR/TE 60.48/1.12ms FOV 340× 289 mm2, scan time per slice 2.6 s, temporal resolution 60.48ms, TPAT factor 4.
Image analysis: For quantitative analysis, LV global myocardial longitudinal strain (GLS), LV circumferential strain and radial strain (GCS and GRS) were measured by dedicated software (QStrain version 2.1, Medis, Leiden, the Netherlands), LV volumes and function were measured using Argus software (Siemens Healthcare, Erlangen, Germany). Specifically, GLS was calculated from 4-chamber, 3-chamber and 2-chamber orientations. GCS and GRS were calculated in the short axis orientation. LV volumes and function were measured in the short axis orientation. Besides, apparent contrast-to-noise ratio (CNR) between LV myocardium and blood pool was also calculated. For qualitative analysis, two radiologists subjectively scored the image quality (IQ) using a four-point grading scale (1=very good IQ, no artifacts affecting cardiac anatomy; 2=good/average IQ, artifacts slightly interfering with cardiac anatomy; 3=below-average IQ, artifacts moderately affecting cardiac anatomy; 4=poor IQ with artifacts severely affecting cardiac anatomy) (1). Wilcoxon signed-rank test was used to compare the measured samples between the conventional method and optimized TPAT technique in both patient groups with/without arrhythmia.
Results
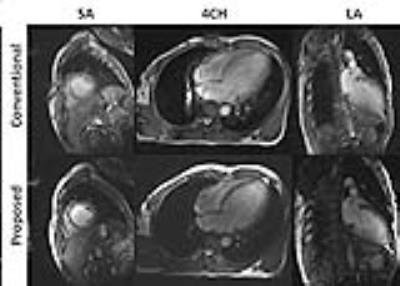
There was no significant difference between the conventional method and TPAT technique in evaluation of LV volumes and function (left ventricular end diastolic volume, EDV; left ventricular end systolic volume, ESV; left ventricular ejection fraction, LVEF; left ventricular stroke volume, LVSV; left ventricular cardiac output, LVCO and Mass), it’s also the same for longitudinal, circumferential and radial strains in both patient groups (Table 1). For the images of patients with arrhythmia obtained by TPAT technique, there were 6 cases of grade 1 (46%), 6 cases of grade 2 (46%) and 1 case of grade 3 (8%), while for those obtained by conventional method, there were 4 cases of grade 2 (31%), 8 cases of grade 3 (62%), and 1 case of grade 4 (7%). The IQ of TPAT technique was higher than that of conventional method in patients with arrhythmia on the whole. (Figure 1). The CNR values in patients with arrhythmia obtained by TPAT were significantly higher than those by conventional method. (10.0±3.4 vs 8.2±2.4, p = 0.009).Discussion
For subjects with normal heart rhythm, there were no obvious difference in CNR of images in TPAT and conventional methods. However, the IQ of conventional method was higher than that of TPAT. For patients with arrhythmia, CNR of images in TPAT sequence was higher than conventional cine sequence. No matter in subjects with normal heart rhythm or patients with arrhythmia, there were no significant differences between conventional and optimized TPAT methods in LV volumes, function as well as longitudinal, circumferential, radial strains. Nevertheless, TPAT can be performed on patients without need of breath holding and use of ECG triggering, which has greater clinical significance than conventional method.Conclusion
With the optimized TPAT technique, the cardiac cine can provide better image quality and shorter scan time in arrhythmia in this preliminary study. Nevertheless, it has the potential advantages of allowing free-breathing scans.Acknowledgements
This work was supported in part by Capital Health Research and Development of Special (2016-4-2063) and Natural Science Foundation of China (81671647).
References
1.Kaasalainen T. Cardiac MRI in patients with cardiac pacemakers: practical methods for reducing susceptibility artifacts and optimizing image quality. Acta Radiol. 2016 Feb;57(2):178-187.Figures