2880
Improvements in Cardiac MR Elastography Using Reduced FOV Techniques1Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Single-shot spin-echo EPI (SS-SE-EPI) has been utilized for cardiac MR Elastography (cMRE) due to its fast imaging speed and insensitivity to cardiac motion. However, the long echo train in SS-EPI makes it vulnerable to image distortion, which can be prominent in cMRE due to the large susceptibility gradient present at the heart-lung interface. In this study, a reduced phase FOV (rFOV) technique combined with a 2D selective excitation has been implemented in the cMRE. And the results showed that the MRE image quality was improved with reduced image distortions and higher SNR.
Introduction
Cardiac magnetic resonance elastography (cMRE) has the potential to become a valuable noninvasive imaging tool for assessing the biomechanical properties of myocardial tissue1. Single-shot spin-echo EPI (SS-SE-EPI) is being utilized for cardiac MRE due to its fast imaging speed and insensitivity to cardiac motion2. However, the long echo train in SS-EPI makes it vulnerable to image distortion, which can be prominent in cMRE due to the large susceptibility gradient present at the heart-lung interface. In addition, full k-space coverage is required for MRE phase-sensitive images, thus partial-Fourier acquisitions are not an option, leading to prolonged echo times and SNR loss compared to conventional magnitude-only cardiac MRI. Earlier studies have shown that combining a 2D selective excitation and a reduced phase FOV (rFOV) is an effective approach for abdominal MRE to shorten the echo train and reduce image distortions without having aliasing artifacts3. The rFOV technique may be particularly well suited for a targeted region such as the heart. The purpose of this study is to demonstrate the improvement in cMRE image quality possible utilizing rFOV techniques.Method
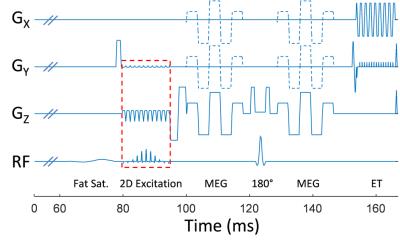
In this study, we used a particular 2D echo-planar excitation RF pulse design4 in which the side excitation bands were tilted away from the imaging volume to avoid unwanted saturation of nearby slices. The 2D RF pulse was implemented into a SS-SE-EPI MRE sequence with moment-nulled motion-encoding gradients oscillating at the same frequency as the external vibration (Fig. 1). A 100-ms pre-encoding time was added before the start of motion-encoding gradients (MEGs) to allow the harmonic motion to approach a steady state after each cardiac trigger. During this waiting time, a fat-saturation pulse was added to suppress the fat signal. Volunteer scans were conducted on a clinical 1.5T GE scanner with an 8-channel cardiac phased-array coil. The vibrations were generated using a high-power active driver and a customized passive drum driver for the heart1. Both full-FOV and rFOV cMRE were performed in an oblique imaging plane to obtain short axis images of the heart using 140-Hz excitation, two MEG pairs, three motion-encoding directions plus one no-motion scan, and four phase offsets spaced evenly over one period of vibration. The TR was matched to the volunteer’s heart rate with peripheral pulse gating. Other imaging parameters included TE = 77.1 ms and 68.5 ms, FOV = 32 x 32 cm2 and 32 x 16 cm2, matrix = 64 x 64 and 64 x 32 for full-FOV and rFOV, respectively; 5 slices across 5 RR intervals; slice thickness = 5 mm; and a parallel imaging acceleration factor of 1. MRE postprocessing involved taking the curl of the 3D displacement field and performing a 3D direct inversion of the Helmholtz equation as described previously1Results
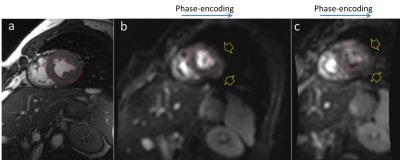
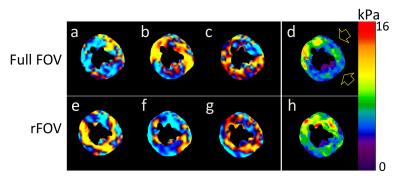
In order to compare the distortion of MRE images, the epicardial and endocardial contours were first drawn on a short-axis FIESTA image prescribed in the same location (Fig. 2a), and then transferred onto the MRE full-FOV and rFOV magnitude images (Fig. 2b-c, respectively). By using rFOV, the distortion was reduced noticeably at the heart-lung interface (yellow arrows in Fig. 2) The SNR was also improved due to the shorter echo time. Fig. 3 shows the X (a, e), Y (b, f), and Z (c, g) components of the curl of the wave fields and the corresponding stiffness maps (d, h) from the full-FOV (top row) and rFOV (bottom row) acquisitions in Fig. 2. Note that the stiffness was underestimated in the areas with large distortion present on the MRE magnitude images (yellow arrows).Discussion
We have demonstrated that reduced-FOV cMRE is a feasible method for measuring the stiffness of the human heart in vivo. Reduced distortions and shorter echo times were achieved by restricting the excitation FOV and shortening the readout echo train. Although using higher parallel imaging acceleration factors can also help reduce distortion, the larger geometric factor (g-factor) will increase the noise amplification, especially around the heart, which is far away from the coil elements.Conclusion
This study demonstrated that SS-SE-EPI utilizing reduced-FOV techniques is valuable in reducing distortion and improving image quality for cardiac MRE. Further validation on cardiac patients will help our understanding of the potential clinical benefits reduced-FOV cMRE can provide for various cardiovascular diseases.Acknowledgements
No acknowledgement found.References
1. Arani, A., Glaser, K. L., Arunachalam, S. P., Rossman, P. J., Lake, D. S., Trzasko, J. D., Manduca, A., McGee, K. P., Ehman, R. L. & Araoz, P. A. In vivo, high-frequency three-dimensional cardiac MR elastography: Feasibility in normal volunteers. Magn Reson Med, (2016).
2. Glaser, K. J., Manduca, A. & Ehman, R. L. Review of MR elastography applications and recent developments. J Magn Reson Imaging 36, 757-774, (2012).
3. Ozaki, M., Arai, K., Miyoshi, K., Worters, P. W., Banerjee, S., Guidon, A., Ikeda, H. & Kabasawa, H. MR Elastography using SS-SE-EPI with reduced FOV for Kidney: Preliminary Study. ISMRM, (2014).
4. Sui, Y., Damen, F. C., Xie, K. & Zhou, X. J. Image domain segmented diffusion imaging using a 2D excitation RF pulse for distortion reduction. ISMRM, (2014).
Figures