2864
The diagnostic accuracy of cardiac magnetic resonance imaging for the differential diagnosis between the left ventricular non-compaction and the negative heart remodeling in thalassemia intermedia patients1Fondazione G. Monasterio CNR-Regione Toscana, Pisa, Italy, 2Università degli Studi di Palermo, Policlinico "Paolo Giaccone", Palermo, Italy
Synopsis
The Grothoff's criteria should be used in the clinical practice in order to improve the specificity of the diagnosis of LVNC and distinguish LVNC and negative heart remodeling in β-TI.
Purpose
The aim of our study was to investigate the diagnostic accuracy of cardiac m)agnetic resonance imaging for the differential diagnosis between the left ventricular non-compaction (LVNC and the negative heart remodeling in β-Thalassemia intermedia (β-TI) patients.
In particular we verified whether the diastolic non-compacted to compacted myocardium (NC/C) ratio criterion could actually discriminate the abnormal trabeculations observed in β-TI from LVNC patients and we compared this diagnostic approach with the CMR criterion suggested by Grotoff M et al.1, which has been reported to be highly sensitive and specific for the LVNC diagnosis.
Methods
CMR images were acquired (1.5 T MR scanner) in 180 patients with β-TI consecutively enrolled in the Myocardial Iron Overload in Thalassemia (MIOT) Network2 and 27 patients with proved diagnosis LVNC studied at FTGM MRI Lab in Pisa from 2002 to 2014.
Cine steady-state free precession sequences were acquired on long-axis two-chamber, four-chamber, three-chamber and short-axis views to cover the whole LV without any gap between images. Cine images were transferred to a dedicated workstation. For evaluation of NC/C ratio, a 16-segment model of the LV3 applied to the three long-axis views was used. At each segment, the thickness of the non-compacted and the compacted myocardium was measured perpendicular to the long-axis direction of the compacted myocardium at end-diastole and the NC/C ratio was calculated. The maximal NC/C ratio was then used for diagnosis. Compacted and global LV mass were measured at the end-diastole. For compacted mass assessment, the endocardial border was drawn to include papillary muscles and exclude trabeculations, while for global mass evaluation papillary muscles and trabeculations were both included.
The CMR diagnostic criteria applied in β-TI patients were: a modified CMR Petersen’s criterion4 proposed by Piga et al5 based on a more restrictive ratio of diastolic NC/C >2.5 at a segmental level and the Grothoff's criteria (percentage of trabeculated left ventricular myocardial mass ( LV-MM) ≥25% of global LV mass and a total LV-MMI NC ≥15 g/m2).1
In the 27 patients with LVNC the final diagnosis was performed based on Grothoff’s criteria and on the clinical/functional criteria for LVNC to further increase the pre-test probability of the disease.
For the calculation of biventricular function, cine Images were analyzed accordingly to a standardized protocol using MASS® software (Medis, Leiden, The Netherlands).6
To detect the presence of myocardial fibrosis, LGE short-axis images were acquired 10-18 min after Gadobutrol (Gadovist®; Bayer Schering Pharma; Berlin, Germany) intravenous administration at the standard dose of 0.2 mmol/kg. Also, vertical, horizontal, and oblique long-axis views were acquired. The extent of LGE areas was quantified using a semiautomatic, previously validated software.7
Results
In β-TI patients at least 1 positive NC/C segment was found in 17 patients (9.4%).
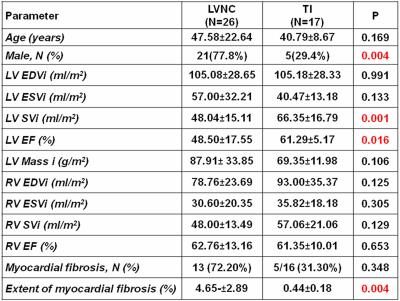
The comparison between LVNC patients and β-TI patients with at least 1 positive NC/C segment is shown in table 1: a statistically significant difference was found in the left ventricular ejection fraction and stroke volume index, lower in patients with LVNC. Although the frequency of myocardial fibrosis was comparable between the two groups, a significantly higher percentage of LGE was found in LVNC patients.
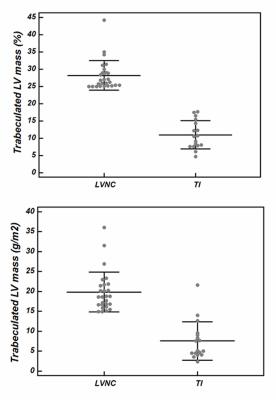
Compared to LVNC patients, in 17 β-TI the mean number of segments with non-compaction areas in every patient were less frequent (5.48±2.26 vs 2.41±1.33; P<0.0001). The LV-MM NC percentage and LV-MMI NCg/m2 were significantly higher in LVNC than in β-TI patients 28.20±4.27% % vs. 10.99±4.09% P<0.0001; 19.88±5.02% vs. 7.58±4.86%, P<0.0001) (Figure 1). None of the β-TI patients fulfilled the Grothoff's criteria.
Conclusion
Our study showed that marked LV trabecular pattern may be seen in B-TI population, instinctively suggesting the morphological phenotype of LVNC. However, none of these patients showed either familial, clinical or morphological changes supporting the diagnosis of LVNC. In the vast majority of the B-TI patients, a comprehensive clinical and imaging evaluation suggests that the increased trabecular pattern represents a morphologic LV variant.
On this basis, we suggest to use Grothoff's criteria in the clinical practice in order to improve the specificity of the diagnosis of LVNC and distinguish LVNC and negative heart remodeling in β-TI.
Acknowledgements
No acknowledgement found.References
1. Grothoff M, Pachowsky M, Hoffmann J, et al. Eur Radiol. 2012;22(12):2699-2709.
2. Meloni A, Ramazzotti A, Positano V, et al. Int J Med Inform. 2009;78(8):503-512.
3. Cerqueira MD, Weissman NJ, Dilsizian V, et al. Circulation. 2002;105(4):539-542.
4. Petersen SE, Selvanayagam JB, Wiesmann F, et al. J Am Coll Cardiol. 2005;46(1):101-105.
5. Piga A, Longo F, Musallam KM, et al. Am J Hematol. Dec 2012;87(12):1079-1083.
6. Aquaro GD, Camastra G, Monti L, et al. J Magn Reson Imaging. 2016; in press.
7. Positano V, Pingitore A, Giorgetti A, et al. J Cardiovasc Magn Reson. 2005;7(2):487-494.