2861
Visualization of atrial septal defects and shunt quantification at multiple locations using 4D Flow MRI in a multicenter pilot study1Erasmus MC, Rotterdam, Netherlands, 2UCSD, San Diego, CA, United States, 3Stanford University, Palo Alto, CA, United States, 4Institute Mutual Montsouris, Paris, France
Synopsis
4D Flow shows clinical promise for a wide variety of cardiovascular applications. We hypothesized that flow measurements may be valuable across a variety of scanning parameters and field strengths typically used in clinical practice. We therefore established a multicenter clinical study at 4 sites using MRI in patients with atrial septal defects. We investigated the consistency of blood flow measurements obtained along the systemic and pulmonary vasculature. Quantitative data appear robust across multiple observers and measurement locations, from data obtained across multiple sites, representing a step forward in the implementation of 4D Flow in clinical practice.
Introduction
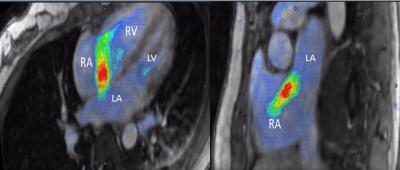
4D Flow is a rapidly evolving MR technique that shows clinical promise with a wide variety of cardiovascular applications, including congenital heart disease. As a volumetric technique, it can simplify acquisition of velocity data while simultaneously visualizing anatomic structures (1–4). Flow can be quantified at any level within the scanned field of view and 4D flow imaging enables calculation of cardiac volumes and biventricular function(3)(5). We hypothesized that flow measurements may be accurately performed across a variety of scanning parameters and field strengths typically used in clinical practice. We therefore established a multicenter clinical study of 4D Flow at sites using MRI for management of patients with suspected atrial septal defects (ASD). We investigated the consistency of blood flow measurements obtained from 4D Flow data at multiple locations along the systemic and pulmonary vasculature by multiple observers.Methods
Results
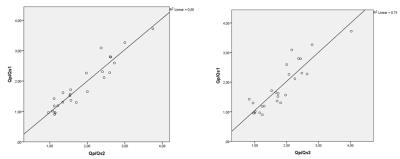
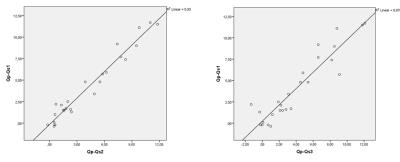
We identified 17 ASD secundum, 2 primum, 2 sinus venosus SVC and 2 sinus venosus IVC. Three of the patients had also PAPVR. Pulmonic flow measured at 3 levels had a mean of 9.25 (+/-4.49), 9.25 (+/-4.44) and 9.25 (+/-4.47) respectively. Systemic flow was 5.15 (+/1.73), 5.10 (+/-1.75) and 5.19 (+/-1.64) respectively. Mean Qp/Qs ratios were 1.83 (+/-0.80), 1.84 (+/-0.74) and 1.80 (+/-0.73). The Pearsons’ correlations between Qp/Qs ratios were very good, with r=0.94 (first and second measurement) and r=0.89 (first and third measurement). Mean shunt volumes at the 3 levels were 4.10 (+/-3.93) l/min, 4.15 (+/-3.74)l/min, and 4.05 (+/-3.84)l/min, and mean direct quantification of the ASD was 3.68 (+/-1.93)l/min. The Pearson’s correlations were r=0.97 (first and second measurement), r=0.93 (first and third measurement) and r=0.82 (first and direct shunt quantification). ICC for inter-observer variability for shunt ratios were 0.92, 0.94 and 0.79.
Discussion
4D Flow provides multiple possibilities for flow quantification (pulmonic and systemic). In the case of aliasing or turbulent flow at a specific level, the clinical question will still be answered by measuring at another location.Conclusions
With this study, we show that 4D Flow is a feasible technique for visualization and quantification of flow volume and shunt volume and fractions. Quantitative data appear reproducible and consistent across multiple observers and measurement locations, from data obtained across multiple sites, which is essential for the implementation of 4D flow imaging in clinical practice.Acknowledgements
No acknowledgement found.References
Bibliography 1. Hsiao A et al. Pediatr Radiol. 2011;41(6):711–720.
2. Hsiao A et al. Radiology. 2012;265(1):87–95
3. Hsiao A et al. 2012;198(3): W250–W259.
4. Vasanawala SS et al. J Magn Reson Imaging. 2015;doi:10.1002/jmri.24856
5. Hanneman K et al. J Magn Reson Imaging. 2016;44(2):383–392
Figures