2859
Quantification of blood flow in the great veins and right heart using 4D flow MRI in Chronic Obstructive Pulmonary Disease: A pilot study in the MESA COPD Study1Department of Radiology, Northwestern University, Chicago, IL, United States, 2Radiology, Northwestern University, Chicago, IL, United States, 3Epidemiology, Columbia University, New York, NY, United States, 4John's Hopkins, Baltimore, MD, United States, 5Radiology, Cornell, New York, NY, United States, 6Radiology and Imaging Sciences, National Institutes of Health, Bathesda, MD, United States, 7Radiology, University of Wisconson-Madison, Madison, WI, United States, 8Radiology, John's Hopkins, Baltimore, MD, United States, 9Radiology, Columbia University, New York, NY, United States
Synopsis
Chronic Obstructive Pulmonary Disease is the third leading cause of death in the United States, and affects 24 million Americans with over 65 million people affected world-wide. Up-to 58% of patients develop exertional pulmonary hypertension and right ventricular volume changes. Understanding this phenomenon, known as cor pulmonale can help us gain insight into the complex pathophysiology involved. This pilot study attempts to apply 4D flow MRI in patients with varying degrees of COPD, and assess the feasibility, reproducibility and accuracy of this technique.
Purpose:
Chronic Obstructive Pulmonary Disease (COPD) is associated with hemodynamic changes in the pulmonary vasculature, potentially resulting in cor pulmonale or right ventricular (RV) hypertrophy, and hyperinflation, potentially leading to underfilling of the RV and cor pulmonale parvis1. 4D flow MRI offers accurate quantification of flow parameters including net flow, peak velocity, and complex flow hemodynamic visualization in the arterial circulation2,3. The ability to retrospectively analyze patients with 4D flow MRI also offers added benefit. This pilot study attempts to assess the feasibility and reproducibility of 4D flow MRI in its application to the great veins and right heart in COPD.Methods:
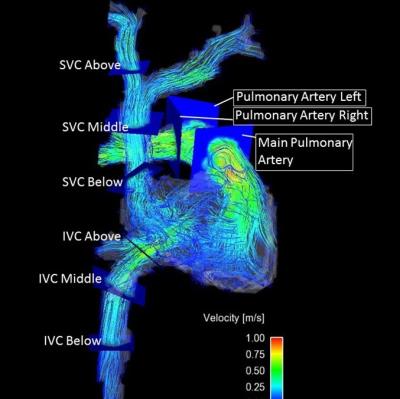
Measurements were performed in the multicenter MESA COPD Study, a nested case-control study of older smokers with COPD and controls. Participants were scanned with 3D time-resolved (cine) radiofrequency spoiled phase-contrast gradient-echo sequence with three-directional velocity encoding (4D flow MRI) at 1.5T Magnetic Resonance (MR) scanner (Siemens Magnetom Aera, Erlangen, Germany). The 4D flow MRIs were read by two observers in 10 patients with COPD and 10 aged matched controls who were blinded to clinical status of the patient. Volumetric coverage included the superior vena cava, inferior vena cava, right atrium, right ventricle, main pulmonary artery, right and left pulmonary arterial branches, and pulmonary veins. Net flow, peak velocity, and retrograde fraction were calculated at each respective area. All data are presented as mean ± SD. Inter-observer and intra-observer reliability were assessed by comparing the net flow metrics generated by two independent observers and by the same observer on two occasions, respectively. Intra-class correlation (ICC) coefficients for both inter- and intra-observer reliability were calculated using one-way ANOVA with random effects in entire sample and also separately in cases and controls. Bland-Altman analysis was also used to quantify agreement between the two observers for net flow through pulmonary veins and arteries by studying the mean difference and limits of agreement.Results:
Of study subjects, 55% were men, 55% were white, 34% were African Americans and 16% were current smokers. The mean age was 66.7 ± 6.5 years. The average ICC for intra- observer reliability in entire sample was 0.93, ranging from a low of 0.67 (IVC below the diaphragm) to a high of 0.98 (IVC above the diaphragm). The average ICC for inter- observer reliability was 0.92, ranging from a low of 0.72 (IVC below the diaphragm) to a high of 0.98 (Left PA and Left superior pulmonary vein) (Table 1). Subjects with COPD and control subjects had similar ICC values. Bland-Altman graphs of the arterial and venous results showed good agreement between observers (Figures 1, 2). The flow rates were consistent in the main pulmonary artery (79 mL/cycle ± 20.5), in the left and right pulmonary arteries (summed: 77.2mL/Cycle ± 12.7), across the Tricuspid valve (80.04 mL/cycle ± 28.93), in the superior and inferior vena cava (summed: 81.71 mL/cycle ± 22.81), and the pulmonary veins (summed: 84.9 mL/cycle ± 42.49) illustrating the conservation of flow (Table 1). There were no statistical differences in net flow metrics between cases and controls in this small sample.Discussion
The results of this study demonstrate the feasibility and reproducibility of measuring venous and right-sided arterial net flow using 4D flow MRI in patients with COPD. The consistency of flow quantification and high intra- and inter-observer correlation coefficient indicate reliable and reproducible measurements. While 4D flow MRI still requires longer processing and acquisition time, the potential complex flow visualization in patients with this pulmonary disease could further the understanding of this disease process (Figure 3).Conclusion
In conclusion, 4D flow MRI acquisition in COPD patients is a promising means of measuring net flow through the thoracic vasculature. The similar results and low variability values lends credence to this method, and potential future clinical applications.Acknowledgements
Funding NIH/NHLBI R01-HL093081, R01-HL077612References
[1] Hueper K, Vogel-Claussen J, Parikh MA, et al. Pulmonary Microvascular Blood Flow in Mild Chronic Obstructive Pulmonary Disease and Emphysema. The MESA COPD Study. Am J Respir Crit Care Med 2015;192(5):570-80.
[2] Markl M, Carr M, Ng J, et al. Assessment of left and right atrial 3D hemodynamics in patients with atrial fibrillation: a 4D flow MRI study. Int J Cardiovasc Imaging 2016;32(5):807-15.
[3] von Spiczak J, Crelier G, Giese D, Kozerke S, Maintz D, Bunck AC. Quantitative Analysis of Vortical Blood Flow in the Thoracic Aorta Using 4D Phase Contrast MRI. PLoS One 2015;10(9):e0139025.
Figures