2854
4D-flow-MRI in patients with Fontan circulation for evaluation of pulmonary artery blood distribution1Department of Radiology, University of Munich, Munich, Germany, 2University of Wisconsin - Madison, Madison, United States, 3DZHK German Center for Cardiovascular Research, Munich, Germany, 4Department of Pediatric Cardiology and Pediatric Intensive Care, University of Munich, Munich, Germany
Synopsis
4D-flow-MRI can serve as a non-invasive imaging modality to monitor patients with congenital heart disease and status post surgical repair. Patients with Fontan-circulation need to be followed up regularly to identify the right time for re-intervention to avoid pulmonary hypertension or atrophy due to hyper- or hypoperfusion, respectively and the development of protein-losing enteropathy.
Introduction
In patients with the diagnosis of hypoplastic left heart syndrome (HLHS) or a single ventricle a so-called Fontan (FO)-circulation is created within several surgical steps to assure viability. At about three years of age the FO-circulation is completed with a Glenn-shunt re-routing blood from the superior vena cava to the right pulmonary artery (RPA) and a FO-tunnel shunting blood from the inferior vena cava directly to the RPA as well, both without a cardiac passage. After pulmonary passage blood runs through a system ventricle towards the aorta. Since patients are growing and nowadays usually reach adulthood regular follow-up has to be performed to monitor the status of the FO-circulation. To overcome the need for regular invasive cardiac catheter the objective of this study was to implement 4D-phase-contrast-flow-MRI (4D-flow-MRI) in the work-up of patients with congenital heart disease and FO-circulation and to evaluate the feasibility to assess and quantify caval blood flow distribution towards the pulmonary arteries (PAs).Methods
4D-flow-MRI scans were acquired with a vendor prototype sequence in 10 FO patients (12,8±4,2 years) with Glenn-shunt and extracardiac tunnel. 4D-flow-MRI was performed with a velocity encoding (VENC) of 100 cm/s, spatial resolution of 2.2x1.8x1.8mm and 10 time-frames/heart beat (HB). Quantitative flow volumes at the level of the Glenn-shunt, the FO-tunnel as well as both PAs were recorded. Flow pattern and distribution to the PAs were visualized using colour-coded path lines. All acquired data were processed offline using vendor prototype software. Results were compared to digital subtraction angiography (DSA) when available.Results
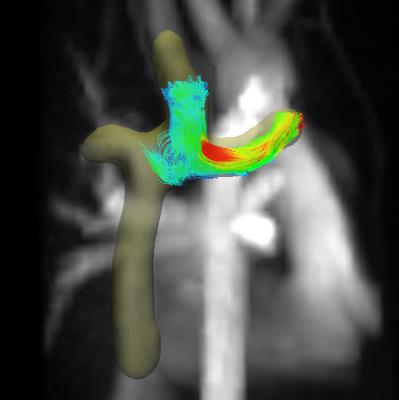
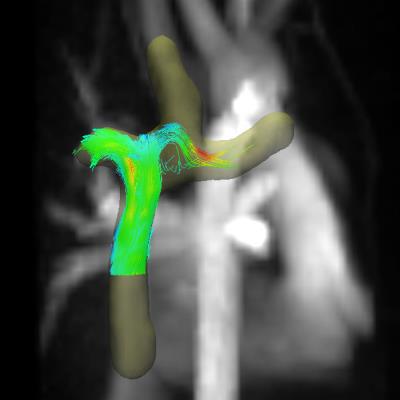
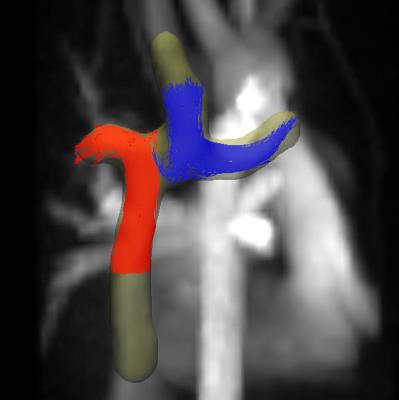
Total blood volume coming from the Glenn-shunt and Fontan-tunnel drained nearly equally to the pulmonary arteries (53% RPA vs. 47% LPA). Left PA blood supply tended to be non-significantly lower but with higher flow velocity compared to the RPA (12,68 ml/HB vs. 15,68 ml/HB; 62,2 cm/s vs 49,7 cm/s), consistent with anatomically smaller or distorted LPAs. Path lines revealed Fontan blood predominantly draining to the RPA in contrast to blood coming from the Glenn-shunt predominantly draining to the LPA. Qualitative flow-pattern results showed good correlation to DSA findings.Discussion
4D-flow-MRI is suitable for regular follow-up exams in patients with congenital heart disease and status post surgical repair. In our group of patients with FO-circulation blood coming from the Glenn-shunt was draining predominantly to the LPA whereas blood coming from the Fontan-tunnel was lead towards the RPA. This is contrary to recently published data, however, within our group Glenn-shunt and FO-tunnel were rather placed orthogonal to each other than with a distinct offset to one or the other side as reported by others.Conclusion
4D-flow-MRI in Fontan patients is feasible with promising results offering a non-invasive method for monitoring patients with congenital heart disease and surgical repair. This work can serve as pilot data for further studies with larger patient numbers to correlate different surgical methods to the resulting PA blood flow distribution and its possible impact on late complications of the Fontan operation like protein-losing enteropathy.Acknowledgements
No acknowledgement found.References
Evaluation of blood flow distribution asymmetry and vascular geometry in patients with Fontancirculation using 4-D flow MRI. Jarvis K, Schnell S, Barker AJ, Garcia J, Lorenz R, Rose M, Chowdhary V, Carr J, Robinson JD, Rigsby CK, Markl M. Pediatr Radiol. 2016 Oct;46(11):1507-19
Geometric characterization of patient-specific total cavopulmonary connections and its relationship to hemodynamics. Tang E, Restrepo M, Haggerty CM, Mirabella L, Bethel J, Whitehead KK, Fogel MA, Yoganathan AP.JACC Cardiovasc Imaging. 2014 Mar;7(3):215-24
Figures