2838
Comprehensive Noninvasive Hemodynamics Using High Temporal Resolution Phase Contrast MR Imaging1Centre for Cardiovascular Imaging, University College London, London, United Kingdom, 2Adult Congenital Heart Disease Department, St Bartholomew’s Hospital, London, United Kingdom, 3IBiTech-bioMMeda, iMinds Medical IT, Ghent University, Gent, Belgium
Synopsis
Implementation of an imaging based technique to perform a non-invasive, comprehensive hemodynamic assessment, using high temporal resolution phase contrast imaging.
Introduction
We have developed a novel cardiovascular magnetic resonance (CMR) protocol that allows comprehensive assessment of central aortic hemodynamics using high temporal resolution phase contrast imaging. Using this approach we derived central aortic systolic blood pressure (cSBP), resistance, compliance, pulse wave velocity and wave reflections, from data acquired in a single breath hold. High temporal resolution imaging is necessary to resolve important wave reflection events in the circulation, which are very short-lived. We investigated this protocol in patients with repaired coarctation of the aorta (CoA) and matched controls. The main aims of this study were i) assess feasibility of the protocol, comparing physiological results with a 1D vascular model of repaired coarctation, ii) characterize hemodynamic differences between patients and controls, and iii) Identify possible biomarkers amongst covariates associated with LV mass (LVM).Methods
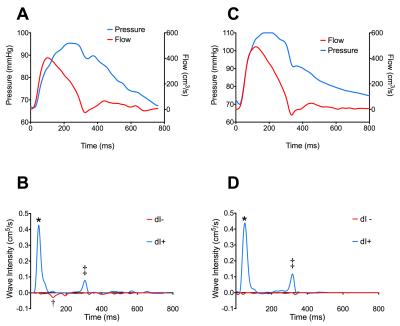
75 subjects, 50 CoA patients, median age 24years (70% male) and 25 matched controls; 23years (72% male) were recruited. Ascending aorta area and flow waveforms were obtained using a high temporal resolution phase-contrast MR flow sequence above the aortic sinotubular junction. The sequence was a prospectively triggered, spiral, velocity encoded spoiled gradient echo acquisition, accelerated with SENSE (TE/TR: 1.9/4.8ms, FOV: 400×400×6 mm, matrix: 192×192, spiral interleaves: 60, SENSE factor: 4, VENC: 180cm/s). The temporal resolution was 9.6msec, the spatial resolution was 2.1×2.1mm and the breath-hold was approximately 11s (16 R-R intervals).1 Oscillometric brachial blood pressure was acquired simultaneously to flow measurements. Ascending aorta area waveforms were used to derive cSBP using an exponential model of the pressure-area relationship calibrated to mean and diastolic brachial blood pressure.2 Total arterial compliance was estimated by parameter optimization of a 2-element Windkessel model. Flow volume (Q) and area curves (A) were used to measure wave reflections in the ascending aorta using non-invasive wave intensity analysis.3 Wave Intensity (dI) is defined as, dI=dA x dQ and dI(±)= ± c/4 [dA ± dQ/c]2 where, c=wave-speed. A validated 1d model of the systemic vascular tree was used to explore differences in wave reflection between controls and patients following coarctation repair. 4 LVM was measured using a short axis stack of cine images.Results
Central SBP was significantly higher in patients compared to controls, 113 (110-117mmHg) vs 107 (103-111 mmHg), [mean (95% confidence interval)], p=0.01. However, there was no significant difference in peripheral systolic blood pressure 122 (118-115mmHg) vs 117 (112-121mmHg), p=0.1. Patients had marked differences in conduit vascular hemodynamics compared to controls: characterized by reduced arterial compliance (p=0.0004) and increased pulse wave velocity (p=0.04). Wave intensity analysis revealed the presence of a midsystolic, backwards compression wave (BCW), figure. The magnitude of the BCW was significantly higher in patients (10e-4cm5 [8e-4 – 14 e-4cm5]) compared to controls (7e-4cm5 [5e-4 - 9e-4cm5]), (p=0.01). These findings were concordant with data from the 1D model, which also demonstrated the presence of a BCW, which increased in magnitude with stiffening of the coarctation repair site. LVM index was significantly higher in patients than controls 72 (68-76) vs 59 (55-63) g/m2, p<0.0005). The elevated backwards reflection wave was found to be an independent predictor of LVM (p=0.01) after adjustment for body size, age and sex.Conclusion
Non-invasive assessment of arterial hemodynamics by CMR is feasible. The use of high temporal resolution flow imaging provides the necessary sampling frequency to measure short-lived hemodynamic phenomena in patients. Using these techniques we have shown elevated cSBP and abnormal vessel stiffness in patients after coarctation repair. Uniquely, we have demonstrated noninvasive measurement of abnormal wave reflections in coarctation repair, which appear to be an important determinant of increased LVM.Acknowledgements
No acknowledgement found.References
1. Steeden JA, Atkinson D, Hansen MS, Taylor AM and Muthurangu V. Rapid flow assessment of congenital heart disease with high-spatiotemporal-resolution gated spiral phase-contrast MR imaging. Radiology. 2011;260:79-87.
2. Quail MA, Steeden JA, Knight D, Segers P, Taylor AM and Muthurangu V. Development and validation of a novel method to derive central aortic systolic pressure from the MR aortic distension curve. J Magn Reson Imaging. 2014;40:1064-70.
3. Quail MA, Knight DS, Steeden JA, Taelman L, Moledina S, Taylor AM, Segers P, Coghlan JG and Muthurangu V. Non-Invasive Pulmonary Artery Wave Intensity Analysis in Pulmonary Hypertension. Am J Physiol Heart Circ Physiol. 2015;308:H1603-H1611.
4. Reymond P, Bohraus Y, Perren F, Lazeyras F and Stergiopulos N. Validation of a patient-specific one-dimensional model of the systemic arterial tree. American Journal of Physiology - Heart and Circulatory Physiology. 2011;301:H1173-H1182.
Figures