2820
Visibility of the draining location of the thoracic duct to the venous system on balanced turbo field echo with extended k-space sampling1Radiology, Tokai University School of Medicine, Isehara, Japan, 2Radiology, Tokai University Hospital, Isehara, Japan
Synopsis
The knowledge regarding the visibility of the thoracic duct draining to the venous system has remained sparse. We assessed the visibility of draining location of the thoracic duct to the venous system in the subclavian region using balanced turbo field echo (bTFE) with extended k-space sampling. As a result, a relatively good visibility was achieved in the thoracic duct and the venous branches in the region. This sequence may be useful to grasp the draining location of the thoracic duct to the venous system at the subclavian region.
PURPOSE
The thoracic duct is the center lymphatic vessels from the cisterna chyli usually to the jugulovenous angle. It can be non-invasively visualized with recent magnetic resonance imaging (MRI) technique, known as MR thoracic ductography (MRTD). A use of balanced turbo field echo (bTFE) sequence on MRTD can visualize not only the thoracic duct, but the surrounding structures such as the arteries and veins.1 Therefore, MRTD with bTFE may also depict the draining portion of the thoracic duct to the venous system at the subclavian region. However, this visibility has not been well understood. Such knowledge will be useful before surgery in this region as well as embolotherapy of the thoracic duct through the subclavian vein.2 The purpose of this study was to assess the visibility of the thoracic duct to the venous system on MRTD with bTFE.METHODS
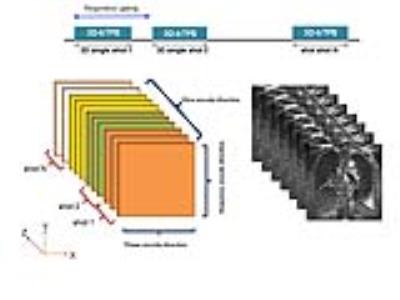
Consecutive 143 patients with esophageal cancer underwent MRTD before surgery. Ten patients were excluded because a part of the subclavian region was outside of the scanned area. Thus, total 133 patients (mean age, 68.0; age range, 26–84) were included in this study. MRTD was performed with a 1.5T MRI (Achieva Nova Dual or Ingenia; Philips, Best, The Netherlands) with a 32-channel-torso-cardiac coil (Achieca Nova Dual) or a 32-channel-torso-coil (Ingenia). MRTD was obtained with 3D bTFE with extended k-space sampling1 (Fig.1) with the following parameters: repetition time/echo time = 5.9/2.9 ms; flip angle = 120 degrees, matrix = 208 × 208, slice thickness = 1.6 mm overcontinuous slices with 50% slice overlapping; turbo factor (number of data sampling per shot) = 200, field of view = 350 mm, SENSE factor = 2, the number of slices = 100, and number of acquisitions = 1; data for total 3D k-space on this sequence was segmentally sampled with respiratory gating. The data were reconstructed to real image to suppress the fat tissue.3 The total acquisition time for MRTD was approximately 2–3 minutes, depending on the respiratory gating. MRTD were retrospectively reviewed by two experienced radiologists with consensus. First, the draining location to the venous system was classified as follows: internal jugular vein, jugulovenous angle, subclavian vein, and others. In addition, the draining site was noted if this was mainly single or multiple. Simultaneously, confident level for visibility of the draining location was evaluated as follows: absolutely certain, somewhat certain (less visibility of the draining portion or less visibility of the continuity from the main thoracic duct), and uncertain.RESULTS
The draining location included the internal jugular vein in 6 patients, jugulovenous angle in 91, left subclavian vein in 18, right subclavian vein in 2, internal jugular vein and jugulovenous angle in 1, jugulovenous angle and subclavian vein in 3, subclavian vein and external jugular vein in 1, and the external jugular vein in 1 (Figs.2–4). In 10 patients (7.5%), the draining location of the thoracic duct was uncertain, whereas, confident level was absolutely certain in 98 (73.7%), somewhat certain in 25 (18.8%). The draining site was identified as multiple in 44 patients.DISCUSSION
We found overall good visibility of the draining location of the thoracic duct in the venous system on bTFE with extended k-space sampling. The majority of the draining location of the thoracic duct were jugulovenous angle, followed by left subclavian artery, and internal jugular vein. In addition, multiple draining sites were found in a certain rate of the patients. MRTD has been mainly performed with single shot heavily T2-weighted spin-echo sequence. However, a use of bTFE shows not only the thoracic vein, but also surrounding vessels. This should be useful to grasp the anatomical location of the thoracic duct in the surrounding structures. In addition, extended k-space sampling combined with bTFE might have reduced the scanning time, allowing an adoption in clinical practice. On the other hand, there were cases with poor visualization of the draining location of the thoracic duct in this study. This seems to attribute to inadequate respiratory gating resulting in motion artifact, or inadequate shimming resulting in insufficient fat-suppression.CONCLUSION
MRTD with bTFE with extended k-space sampling can relatively well depict the draining location of the thoracic duct to the venous system in the subclavian region.Acknowledgements
No acknowledgement found.References
1. Nomura T, Niwa T, Kazama T, et al. Balanced turbo field echo with extended k-space sampling: a fast technique for the thoracic ductography. Magn Reson Med Sci. 2016,15(4):405-410.
2. Koike Y, Hirai C, Nishimura J, et al. Percutaneous transvenous embolization of the thoracic duct in the treatment of chylothorax in two patients. J Vasc Interv Radiol. 2013,24(1):135-137.
3. Hargreaves BA, Vasanawala SS, Nayak KS, et al. Fat-suppressed steady-state free precession imaging using phase detection. Magn Reson Med. 2003,50(1):210-213.
Figures

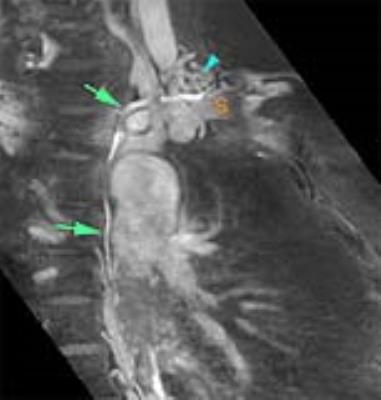
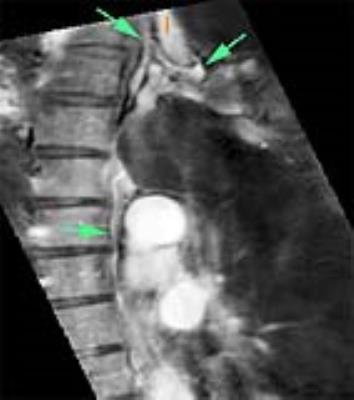
Magnetic resonance thoracic ductography (MRTD) with balanced turbo field echo with extended k-space sampling in a 68 year-old female. MRTD with partial maximum intensity projection well visualize the thoracic duct (arrows) draining to the jugulovenous angle.
I: internal jugular vein, S: subclavian vein