2818
Clinical utility of the pulmonary artery to ascending aortic ratio by cardiac magnetic resonance in patients with pulmonary hypertension.1Diagnostic and Interventional Radiology, Hokkaido University Hospital, Sapporo, Japan, 2Nuclear Medicine, Hokkaido University Hospital, 3First Department of Medicine, Hokkaido University Hospital, 4Department of Cardiovascular Medicine, Hokkaido University Hospital
Synopsis
Thirty-three patients with pulmonary hypertension (PH) and age-, sex-matched 15 controls were retrospectively evaluated. The pulmonary artery to ascending aortic ratio (PA-A ratio) measured by cardiac MRI was significantly higher in PH patients than that in controls. The patients with pulmonary arterial hypertension showed a significantly higher PA-A ratio compared to patients with other causes of PH. Increased PA-A ratio showed significant correlations with right ventricular (RV) dilatation and decreased RVEF. The PA-A ratio showed high sensitivity and specificity for detection of PH. The PA-A ratio using cardiac MRI is an easy surrogate marker for detection of RV dysfunction and PH.
PURPOSE
Cardiac magnetic resonance imaging (CMRI) can quantify right ventricular (RV) volumes, ejection fraction and provide morphological information such as diameters of great vessels1. Wells et al. reported that increased size of the pulmonary artery could be the result of pulmonary hypertension2. Relative pulmonary artery enlargement, as determined by a pulmonary artery to ascending aortic ratio (PA-A ratio) may identify patients with pulmonary vascular disease2,3. The aim of this study was to investigate the diagnostic power of the PA-A ratio by CMRI in PH patients. We correlated the PA-A ratio with RV functional parameters (RV end-diastolic volume (EDV), end-systolic volume (ESV), and ejection fraction (EF)) and the results of right heart catheterization (RHC).METHODS
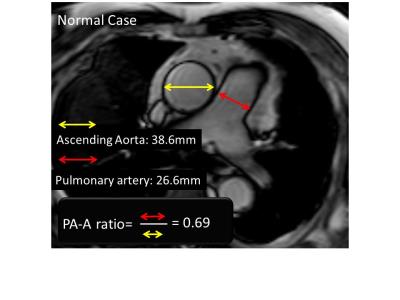
The institutional review board approved the retrospective study and waived the requirement for informed consent. Thirty-three patients (9 males, age 57±16 years old) with PH (mean pulmonary artery pressure (PAP) >25 mmHg) between December 2009 and September 2015 were enrolled in this study. CMRI was performed as a part of clinical routine. Fifteen age and sex matched patients with normal RV function (RVEF ≧ 45%) and no cardiac disease (no late gadolinium enhancement and pulmonary hypertension) were enrolled as the control group. CMRI was performed with a 1.5 T whole body scanner Achieva (Philips Medical System, Best, The Netherlands), equipped with a 32-channel phased-array coil. Functional cardiac imaging including trans-axial and left ventricular short axis planes was performed by breath-hold segmented k-space steady-state free precession (SSFP) techniques (TR/TE/FA, 3.5/1.75 ms/ 60°; spatial resolution, 2.97×2.86×8mm; slice thickness 10mm; matrix: 128×108; 20phases). All CMRI measurements were performed by a blinded cardiovascular radiologist unaware of the RHC results using View Forum (Extended MR Work Space: ver. 2.6.3; Philips Medical Systems, Best, The Netherlands). Pulmonary artery and ascending aortic diameters were determined from inner-edge to inner edge in trans-axial SSFP end-diastolic phase at the level of the PA bifurcation. Representative images of the pulmonary artery and aortic measurements are given in Fig.1 and 2. LV and RV endocardial borders were semi-automatically traced from the stack of cine images to obtain EDV and ESV. RHC was performed within 2 weeks in patients with PH. In controls, 13 patients underwent echocardiography instead of RHC and systolic PAP was estimated. One-way ANOVA was used to test the differences in RV volume parameters and the PA-A ratio between the PH and control groups. The PH group was also divided into pulmonary arterial hypertension/pulmonary veno-occlusive disease (PAH) and other PH groups (lung PH and chronic thromboembolic PH). Differences in the PA-A ratio among different groups were assessed by Tukey-HSD test. Correlations between the PA -A ratio and results of RV volume analysis and RHC were evaluated by linear regression analysis. Sensitivity and specificity of the PA-A ratio and a diameter of pulmonary artery for detection of PH was verified by a ROC-curve analysis. All statistical analyses were performed using JMP 12.0.1 (SAS institute, Cary, NC, USA).RESULTS
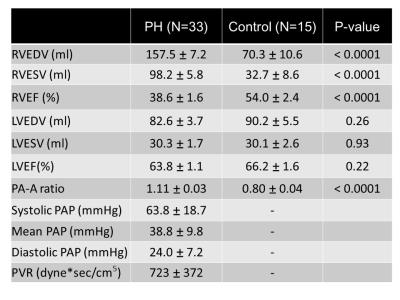
Results of CMRI and RHC are summarized in Fig.3. RV volumes and RVEF differed between the PH and controls (p<0.0001 for all), while LVEF did not differ between groups (p=0.12). The PA-A ratio in PH patients (1.11 ± 0.03) was significantly higher than that in controls (0.80 ± 0.05) (p<0.0001). The diameter of PA (31.7 ± 0.8mm) was significantly larger in PH than that in controls (23.9 ± 1.2mm) (p<0.0001), while there was no such difference in the aortic diameter (p=0.28).
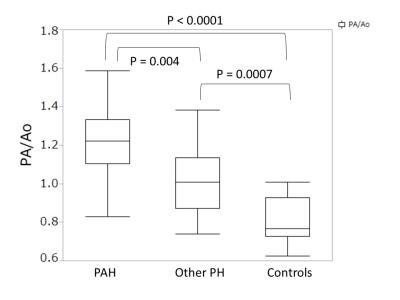
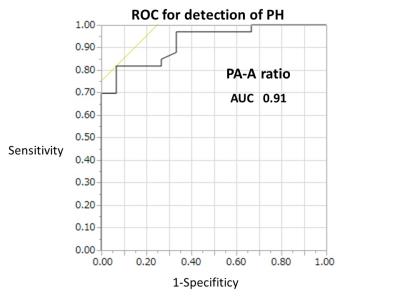
In 33 PH patients, 16 patients (48%) were diagnosed as PAH. The PA-A ratio in the PAH group was significantly higher than those in other PH and control groups (Fig.4). The PA-A ratio presented a significant positive correlation to RVEDV (r= 0.60, p<0.0001), to systolic PAP (r =0.49, p=0.0007), and a significant negative correlation to RVEF (r= −0.43, p = 0.003). The PA-A ratio showed high sensitivity and specificity with 70% and 100% (a cut-off of 1.02, AUC=0.91, p= 0.0005) for detection of PH (Fig.5).
DISCUSSION
The PA-A ratio was significantly higher in PH patients than that in controls. Increased PA-A ratio showed modest correlations with RV dilatation and dysfunction. The PA-A ratio showed high sensitivity and specificity for detection of PH. The PA-A ratio using CMRI is an easy surrogate marker for detection of RV dysfunction and pulmonary hypertension.CONCLUSION
The PA-A ratio determined by CMRI significantly correlated with RV dilatation and dysfunction and might be a good marker for detection of PH.Acknowledgements
NoneReferences
1) Marcu CB, Beek AM, van Rossum AC. Clinical applications of cardiovascular magnetic resonance imaging. CMAJ 2006;175(8):911–7.
2) Wells JM, Washko G, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913-21.
3) Shin S, King CS, Brown AW, et al. Pulmonary artery size as a predictor of pulmonary hypertension and outcomes in patients with chronic obstructive pulmonary disease. Respir Med. 2014;108(11):1626-32.
Figures